The complexity of -interrelated- planet and human health and the lack of international consensus on the sustainability threshold of carbon footprint deserves some analysis and reflection. The Authors hereby relate some concepts and pieces of evidence which alarm on this challenge, most probably Humanity´s greatest this century

By Juan E Garay*, David E Chiriboga, Nefer Kelley, Adam Garay, Estefania Garcia-Carmino
Equity Movement
*Corresponding Author and ad-honorem Professor of bioethics, University of Chiapas, Mexico
Health and Climate Change: a Third World War with No Guns
First published 19th July 2018. Updated 22nd October 2018
For the last 200,000 years (less than 0.02% of time of life on Earth- equivalent to half an hour in one year) we have seen ourselves as “homo sapiens”. Due to our unique sophisticated-crafting activity (as hands are not used for walking) and our abstract thinking (as our frontal lobe grew) we have evolved to believe in our superiority to other forms of life and hence justify understanding nature as the means to satisfy our needs and ever-growing ambitions (driven by the abstract projections). Some 5 generations ago (one thousandth of our time on Earth) we discovered nature’s resources under the surface, the life (carbon) sediments of over 3 billion years. We learnt how to burn them and boost our ambition and “needs” (consumption). In the last two centuries, we have based most of the way we work, we move, we eat, we warm or cool, we relate, we think, in burning our planet’s inner life sediments to “fuel” (and so we call it) our lives. This activity has had such a (destructive) impact in our planet that some call this the planet’s Anthropocene era, after the very stable (weather-wise) 10,000 years of the Holocene. Our generation, around the 5000th, is the most privileged in life expectancy and sophistication in the capacity of transformation of nature to meet our needs, well rather, our abstract-driven ambitions. But the way we have been using Nature has surpassed its capacity to recover in balance to the speed of our damage. We damaged the basis of life as we exhausted soils, dried water sources and cut down the forests. We hence reduced life’s main wealth, its diversity of adapting through the last 3 billion years. We have also upset the balances of hydrogen, phosphorus and nitrogen in the soils and oceans. We have filled the air with the carbon extracted and burnt and upset its balance with oxygen. We have even broken-down elements so they will generate radiations distorting life cycles for thousands of years.
Nature suffers our unbalanced damage but we will suffer it gradually advancing towards our extinction which -if our destructive mode persists- would be a relief for our planet and life in it which would soon (in the Planet’s time dimension) recover from our damage which is, overall, an unconscious and self-centered (narcissistic) suicide.
One of the ways we damage the Planet and progress towards our extinction is by burning underground carbon and releasing it above the surface. All that carbon (more than the natural carbon cycle of the Planet’s surface) is accumulated in the atmosphere. Since the time we started burning coal in the XVIIIth century and later boosted with the burning of liquid oil mainly in the XXth century and gas by this XXIst century, we have released some 700,000 million tons of carbon in the atmosphere surrounding and protecting life in the planet.
The carbon accumulated in the atmosphere is measured by particles per million. Their greenhouse effect traps the solar radiation overheating the Planet’s surface temperature. There is a strong linear relation between the million if carbon tons accumulated in the atmosphere, and Planet`s surface average temperature increase.
As all inter-connected living creatures, including ourselves, the Planet needs a fine equilibrium if its temperature to maintain the complex interaction of molecules we call life. As our life is compromised with fever, so is the Planet`s. And in a very similar range: temperature increases above 2 degrees our average baseline (fever above 38.5 Celsius degrees) compromise our individual health, and so it also happens with life (inclusing ours) in our Planet. The most recent IPCC report brings that threshold lower, to 1.5°.
In the last 200 years, we have caused the Planet (as infections – uncontrolled growth of microorganisms- behave in our body) to suffer progressively of mild fever episodes causing draughts, and consequences of sweating (floods) and possibly even shivering (earthquakes). Those are the fever-related symptoms, while we also cause dehydration (water shortage), alopecia (deforestation), dysbacteriosis – imbalance with our bacteria in the gut mainly, the cause and consequence of most ill health- (loss of biodiversity), tumors (uncontrolled growth of cities), metabolic disorders as diabetes (imbalances of carbon, nitrogen and phosphorus, the players of life, resulting in the acidification of soils and oceans) or intoxications (as heavy metals in lands and plastics in oceans, soon more than fish).
The Planet will survive to this annoying self-centered human infection and recover to a harmony among its living dwellers but we – at this rate- will not only extinct but leave the worst form of life`s legacy proving probably an evolutionary mistake, in the history of our Planet.
Within our homo sapiens time of 30 minute-period-in-year, our generation, a 5-minute glimpse of time in one year, is the most privileged yet the most destructive and will leave the worst legacy ever to our children and grandchildren.
The analysis
We lack knowledge on the depth and width of the consequences of global warming above 2 degrees over the year 1850 baseline. In human health, the estimates based on the impact of vector-borne infections, water restricted-related diarrheal diseases, crops` impact-related malnutrition and heat waves. The analysis by WHO renders an estimate of 250,000 excess annual mortality with 2 degrees increase[1]. While that may sound tragic enough, it only represents a 0,3% increase in mortality and ill health, highly likely a gross underestimate of the impact we`ll suffer from the dramatic and unprecedented climate and environmental change we`re responsible for.
We now have some preliminary evidence of the effects of temperature increase due to human pollution on excess mortality by geo-climatic regions [2]. We have applied the reported excess mortality rates (age, sex and region- specific) under the current trend of growing carbon emissions (despite the Paris agreements- in any case insufficient) to the UN prospects of population and mortality for the rest of the XXIst century by countries according to the Koppen climate classification. The analysis results in 216 million excess deaths due to temperature increase, mainly in the last three decades of the century, in > 65 years of age and in the sub-Saharan and South Eastern Asian regions. A higher disaggregation of sub-national regions would surely render higher sensitivity and a larger death toll due to temperature increase.
This tragic death toll is over three times that of the Second World War. Man-made climate change is a silent Third World War with no weapons, just blind (the worst kind, the one which refuses to see) negligence (as if we were driving without seeing, and constantly killing others…), it mainly kills people with no responsibility in carbon emissions, as 80% of deaths will take place in the non-polluting tropics.
In order to develop better mathematical models to predict the real effect of global warming and the distribution of such impact across populations and territories and hence better estimate the burden of inter-generational inequity, and better understand the major consequences of our lifestyles today in the lives of our children and grandchildren, we are developing intergenerational health equity metrics based to estimate such burden by country, age , sex and time period.
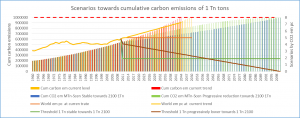
The strong correlation between the cumulative carbon emissions, particles per million and temperature increase, has been clearly proven[3]. The following graph shows the correlation between the models of cumulative carbon emissions and global warming, with a clear crossing of 1000000 million tonnes (one trillion), at 2 degrees excess temperature[4].
Given the dramatic rate of Nature and self-destruction, Humanity needs to change in this century its ways of living, producing, consuming, moving, relating, using energy and developing knowledge and global public goods, in order to avoid the 2 degrees Celsius in excess (fever) of baseline levels in 1850, when this destructive dynamic started.
Such profound changes require at least two generations with generation of conscience, knowledge, attitudes, means and practices, that is, the remains of the XXIst century.
The universal ethical threshold of CO2 emissions
In order to avoid the dramatic glass-roof of 2 degrees increase due to the cumulative 1 trillion tonne carbon emissions, we have calculated the ethical threshold of annual per capita carbon emissions so that all persons foreseen to live during the XXIst century would collectively produce less than the approximately 400,000 tonnes remaining to the trillionth one. Humanity has identified sources of oil and gas which if burnt would mean over 1,2 billion tons of carbon emissions, three times the space to hit the 2º threshold, and yet oil companies worldwide continue to search for more reserves.
Figure 1 shows the predictions of cumulative carbon emissions (in bars) given the UN Population forecast for the century and in four scenarios of annual carbon emission annuals per capita: the present level, the present trend (based on time series of the last 20 years) and the maximum levels which in a stable or progressively lowering trend would avoid the trillion tonne cumulative carbon emissions by year 2100. At the present level of carbon emissions, we would hit the trillion tones (and the consequence of 2 degrees warming) by 2044. Given the slight lowering trend in the last ten years, the present trend of emissions would mean reaching the trillion tones 5 years later, in 2049.
Figure 1 : Calculation of the sustainability threshold of carbon emissions 1960-2100
In a stable way, the ethical universal threshold in Humanity’s main challenge this century is of 1.7 tons of CO2 (3.67 conversion factor from carbon to CO2) per person and year. This is the limit for every human being (in annual CO2 emissions) required to preserve the Planet for our children and grandchildren. We call it the Universal Ethical Threshold (UET). In a progressive lowering rate, it would start from the present world average levels of 5 cross by 2060 the average threshold of 1.7 and thereafter decrease till zero emissions by 2100.
In any scenario, the ethical threshold is calculated as the per capita share given at any time the balance to one trillion tones and the estimated population living in the planet until 2100.
Ethical threshold vs present situation and trend
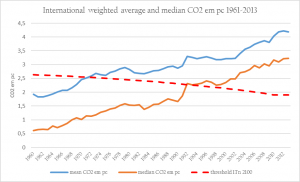
In contrast with the ethical threshold calculated (to spare the coming generation from a tragic global warming with yet unknown impact on human health-even survival as a species-), Figure 2 represents the relation between the ethical threshold of CO2 emissions and the average and median values of global human emissions. The median is lower than the mean given the accumulation of high values in a lower share of countries. As Humanity, we have trespassed this ethical threshold in 1970 and now stand at emissions 2.5 times higher than the universal ethical threshold (UET).
Figure 2: International average CO2 emissions pc vs sustainability threshold, 1961-2013
The number of countries where the average carbon footprint per capita was under the universal ethical threshold (UET) has been decreasing since 1960 going from 140 in 1960 to some 80 now. The present trend points at a continued decrease down to 60. The Paris agreement in Conference of Parties (COP)-21 would reduce the downfall and lead to a stable number till 2030 of some 100 countries (half the world’s nations) below the UET, that is, with sustainable level of carbon emissions which would avoid the trillionth ton glass roof and the 2ºC increase, enabling a chance to shift towards a post-petroleum XXII nd century. The population living in sustainable countries went from 2 billion in 1960 to over 3 billion in 1990 but then fell abruptly (to some 2.5 billion) due to the increase of carbon emissions (surpassing the UET) in China. Under the current trend scenario, the total population under the UET would slowly grow (due to the population growth rate in low income countries) hitting another abrupt decrease in 2020 due to the increase of per capita emissions above the UET in India, going back to some 2 billion living in countries with ecologically sustainable economies, less than one third of the world´s population. If COP 21 commitments are met, India would not fall out of the sustainability group and in fact China would rejoin by 2028, increasing the overall population living in sustainable countries to close to six thousand million people, half the world`s people and over twice the scenarios without the COP 21 commitments.
If the COP-21 commitments are met in 2030, the population entering the countries` sustainability range due to compliance with COP-21 commitments would belong to 13 countries, with 44% of such population from India, 41% from China, 8.5% from Indonesia and 3% from Vietnam (the four latter add to 95% of the additional 3.8 billion people under the UET). The world`s share of population under the UET has a step-ladder shape with slow decrease since the 60s till the 90s (60 to 50%), a first abrupt fall to 35% due to China`s surpass, followed by again slow gradual decrease till 2020 when (under the current trend), India would fall out and the overall share would be around 20%. If COP 21 commitments are met, then, as mentioned above, India would not fall out in 2020 and China would rejoin near 2030 so the final share would be some 50%. Some 50% of the world`s population would be producing some 20% of total emissions (40% and 10% respectively without China before 2028).
2030 scenarios
Three different scenarios may be foreseen towards 2030: the present trend, the one under compliance of COP21 commitments and the former one excluding the USA (given their recent withdrawal). There would be a reduction to less than 50% of the current trend if COP 21 commitments were met by 2030, yet it would still be some 50% higher than the required UET. The withdrawal of the USA (if their current slow-lowering trend) would only (given their moderate COP21 commitments) increase some 0.1% the already too-high world`s average carbon footprint per capita.
In summary, the world runs blind and hastily towards the global warming threshold (fever of the planet) of the 2 degrees excess unprecedented for Human kind. At the current rate and trend, we would reach that turning point (possibly of no return) by the half of the century. By COP 21 commitments emissions would be reduced in 2030 by half of what the present current trend would lead to, and the population living in countries below the UET would double (to half the world’s population), largely due to the commitments of India and China.
The forecast after 2030 depends on whether the current trend remains, the COP 21 commitments remain stable after 2030, their lowering trend continues till 0 or it even goes beyond and starts recapturing the carbon in the atmosphere by knowledge and technology developed for that aim.
Inter-generational inequity
The above analysis reveals a very likely damage to the planet and the environmental conditions affecting the next generation. WHO has only estimated some 0,5% increase in the burden of ill health if we hit the trillion ton and the 2ºC of global warming. Given the major implications of such global warming -unprecedented for the last 200,000 years- in all living factors (nutrition, water, air, temperature) and the already major impact it has in many other living species on earth, it seems that 0,5% impact on our health is a gross underestimate.
References
[1] http://www.who.int/news-room/fact-sheets/detail/climate-change-and-health
[2] https://www.thelancet.com/journals/lanplh/article/PIIS2542-5196(17)30156-0/fulltext.
[3] http://iopscience.iop.org/article/10.1088/1748-9326/11/6/065003/pdf
[4] Myles R. Allenet al, Warming caused by cumulative carbon emissions towards the trillionth tonne, Nature 458, 1163-1166 (30 April 2009)