Summary Since January 2020, official sources reported 360 million COVID 19 infections and 5.6 deaths with COVID-19 infection. While the distribution of mortality has no relation with national average GDP pc, the world has responded a scope of lockdown measures and through the development and distribution of COVID 19 vaccines, with very high degrees of impact on inequity. There are uncertainties in the real incidence (probably much higher than reported) and case fatality rates (probably much lower) and the risk benefit of natural immunity vs. induced immunity by COVID vaccines, disaggregated by age and risk factors. The analysis of the burden of disease (in life years lost) points at 1.9% of the global burden of ill health. The estimated cost-utility (economic cost per life year prevented) of the mentioned preventive measures (lockdown and vaccination) has been much higher than indicative national thresholds in low and middle-income countries. Even in high-income countries, the economic contraction derived from lockdown is above the reference cost-utility thresholds while universal vaccination is very close to the mentioned threshold set in some countries. The opportunity cost of the economic lockdown vs. ethical redistribution is of 4.9 million while that of the overall vaccination is of over 2 million, 2.4 million for those under 60 years of age. The only intervention with no opportunity cost is the vaccination of people older than 60 years and/or with risk factors, which has a net saving effect of close to 0.5 million deaths. This analysis points at COVID 19 equitable vaccination of all persons older than 60 years, regardless the country or income group, as the most efficient and ethical use of the global economic resources to prevent loss of human life due to COVID 19. While vertical and systematic interventions may be pertinent in epidemic contexts (as the evolution in incidence and fatality is unknown), the analysis questions the pertinence of COVID 19 vaccination in people younger than 60 years in a stable endemic situation and in relation to other more cost effective public health interventions lacking coverage in low-income countries
By Juan E. Garay, MD MPH MSc
Co-founder and member of the Steering Committee, Sustainable Health Equity Movement
Professor ad-honorem, UNACH, Chiapas, Mexico, Visiting Professor of Global Health, Escuela Nacional de Sanidad, Spain
COVID-19 IN THE CONTEXT OF GLOBAL HEALTH EQUITY
The study here is an update to a version already published on PEAH
Scene setting
Global health in equity: Equity is the fair distribution of inequality. It is the measure of the only international commitment in global health, Article 1 of the Constitution of the World Health Organisation: “the best possible health for all”. We have defined the best feasible level of health as the one of “HRS” countries or regions with : (1) life expectancy higher than the international average (H: healthy), (2) flow of economic resources (GDP per capita) and wealth (assets) below the international average (R: Replicable in terms of economic resources) and (3) with availability (bio-capacity per capita) and use of natural resources (carbon footprint and ecological footprint) below the ecological sustainability thresholds- or planetary boundaries (S : Sustainable in the use of natural resources)[1].
We compared the mortality rates disaggregated by age and sex with those observed in each country of such HRS references. The excess mortality constitutes the net (number of deaths) or relative (proportion of deaths in excess, from the total) burden of health inequity. Based on available data on national averages, the net burden of inequality between 2016 and 2020 was on average 16.11 million annual deaths and the relative burden, 28 % (32 % for women and 23 % for men)[2]. Eighty four per cent of the net burden/excess mortality (13.53 million deaths) took place in countries with GDP per capita lower than the healthy-replicable-sustainable (HRS) references, which we defined as the ‘dignity threshold’, of around $10.7 per day (5.7 times higher than the ‘poverty threshold’ defined by the World Bank). When we studied the symmetrical level of the dignity threshold GDP pc above the international average we found out that no country with average GDP pc above such level (which we call “excess threshold”) has respected, during 60 years, the planetary boundaries. On the other side, average life expectancy (proxy for wellbeing) does not improve with GDP pc above the excess threshold[3]. More than half of the world’s population live in countries with GDP pc below the dignity threshold (in the deficit area). For them, the average income levels (related to access to knowledge and basic goods) are below those required (dignity threshold) to enable health and life expectancy that is feasible (indeed, with less than half of global economic resources) and sustainable for the next generations, as the WHO constitution states. The economic redistribution needed to ensure all countries have national average GDP pc above the mentioned dignity threshold (and economic conditions to prevent those 13.53 million deaths per year) is equivalent to 7.77 % of global GDP, 10.6 % of the GDP above the excess threshold (as opposed to the current 0.18 % ODA). Regarding the intergenerational prospects of health inequity (between the present one and coming generations), the current CO2 emission trend (after the COVID 19 lockdown emissions returned to their average growth rate) will cause some 220 million excess deaths during the rest of the century, hitting the least polluting countries harder (“exponential inequity”).
COVID-19 and equity: available data point at a distribution of COVID 19 attributed mortality by demographic, geographical and economic factors, as follows:
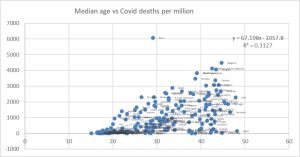
Demographic distribution: Half of all deaths have occurred in patients aged over 85, above the highest national average of life expectancy (Japan, 84.36), two-thirds in patients aged over 80 (above the average of high-income countries), 80 % in patients aged over 72 (above the international average of life expectancy) and 95 % in patients aged over 60 years[4]. That explains the correlation COVID 19 related mortality rate by country and its median age. As the following graph shows, one third of the international variability of COVID 19 mortality could be explained by the median age.
Figure 1: Cumulative mortality 2020-2021 per million per COVID-19 vs median age, by country
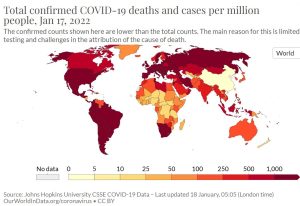
Geographical distribution: The following map shows the distribution of deaths per million by national averages, with higher rates in the Americas, Europe, Russia and Southern Africa Cumulative mortality rate per Covid per national average [5].
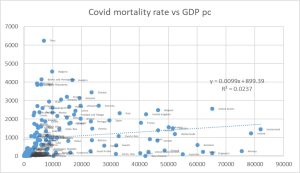
As shown in the graph below, the cumulative mortality rate for COVID-19 is unrelated to the GDP per capita (r2 = 0.023).
Figure 2: Cumulative mortality 2020-2021 per million per COVID-19 vs GDP pc, by country
Reported vs estimated public health COVID 19 indicators
Analysis of the magnitude (and distribution) of the pandemic
Any cause of loss of health (risk factor or disease) is measured in relation to others by incidence (cases/population), fatality (deaths/cases) and the “burden of disease” (healthy life years lost by that cause, in the population).
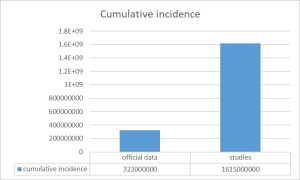
- Incidence: Diseases causing acute infections such as COVID-19 are better measured by regular sero-prevalence studies which allow the estimate of the cumulative proportion of people which have been already infected (with presence of IgG antibodies). During 2020, the pandemic year prior to COVID 19 vaccination, sero-prevalence studies could have estimated the real incidence of the disease. In contrast, the reporting systems varied between countries as they screened either symptomatic cases, serious cases or primary or secondary contacts. Those daily reports of “new infections”, largely biased and non-comparable between countries have received the focus of the media and the attention of societies around the world. Even in the same country, the case detection system varied, so the comparison between pandemic waves is also biased. In the few[6] (and hardly disseminated and discussed) sero-prevalence studies conducted, the real cumulative incidence of the pandemic was between 2 and up to 10 times higher[7] than the officially reported one. Although the official WHO consolidated data show a cumulative incidence of 323 million cases, applying the ratio of sero-prevalence studies/reported cases in the populations thus studied and on a weighted basis (according to population sizes), the real cumulative incidence may be of more than 1,600 million, as shown in Table 1. The distribution of the incidence rate in the population is uncertain due to the lack of population studies, but it seems to have been affecting more young people as the pandemic evolved.
Figure 3: Incidence of COVID-19 data and estimation by sero-prevalence studies
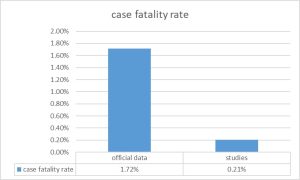
- Case-Fatality: In addition to the underestimation of the cases described above (denominator of case fatality), the number of deaths by COVID-19 was most likely so biased. After two years of pandemic, the question of either death with COVID-19 or death by COVID-19 arises[8]. Following infection or vaccination it seems the virus genome can, by reverse transcriptases, integrate into the human genome and express mRNA (PCR positive) and Receptor Binding Protein (positive antigen test) without the presence of active viruses in the body[9]. On the other hand, even in the presence of active infection (if demonstrated by viral culture), the virus may be asymptomatic or only cause mild (as shown in the sero-prevalence studies described above) symptoms and not be the main or direct cause of severity or death. Most of the deaths attributed to COVID-19 have been in the elderly and with underlying pathologies, any of them potentially also lethal. As the pandemic evolved and affected a larger cumulative proportion of the population, and as other clinical symptoms and signs were attributed to the virus, the proportion of those deaths where the presence of COVID 19 antigen or PCR was either not related to active infection or not the primary or final cause of death may have increased. Therefore, the reported mortality attributed to COVID 19 may have been overestimated. The real mortality rate could only be known by autopsy series, which were rarely performed or published during the pandemic, due to the collapse of the health system itself. In the few unpublished autopsy series, around 40 %[10] of the deaths attributed by COVID-19 were actually due to other causes, in particular the complications of hypertension, obesity and diabetes and undiagnosed cancers. Inversely, there may be countries where there is an under-reporting of mortality in general and of mortality certificates with accurate diagnosis of cause of deaths and the reported COVID 19 mortality rates may be a gross underestimate and explain, partly, the much lower rates in sub-Saharan Africa. As regards the assumptions that there is an underestimation of COVID-19 deaths in relation to the levels of excess mortality above the baseline levels, it is unclear whether it is due to the pandemic effect or the lockdown measures and their multiple health effects, as described below. Taking into account the previously estimated incidence according to population sero-prevalence studies and the mortality adjusted to the proportion of deaths directly caused by COVID-19 among those attributed to it, the case fatality could be as low as 0.33 %, very similar to seasonal flu. The distribution of the case fatality rate in the population is, in any case, very uneven, showing variations from less than 1 per 1,000 cases in under 30 years of age to more than 20 % for patients over 80 years of age. It seems that case fatality of the disease has been decreasing, due to a growing share of infections in the youth, the effects of the pathogenicity of evolving variants (as recently observed in Omicron), the effects of natural and induced immunity and the effectiveness of treatments.
Figure 4: Fatality calculated by official data and estimated by the adjustment of COVID-19 mortality and the highest estimated incidence level
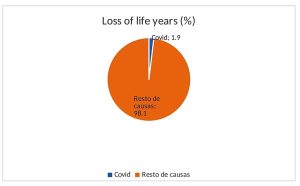
- Burden of disease: The loss of life years is measured in each disease by the difference between the age of death for the cause studied, in this case the COVID-19 infection, and the average life expectancy in a given population[11]. Global comparative studies use as a reference the highest national average life expectancy. As the average age of death has been (according to studies in the United States) 71.63 years, the average each death by COVID-19 has caused the loss of 12.73 life years in relation to the mentioned reference. As the cumulative number of deaths has been around 5.12 million in 2020-2021, the pandemic has caused the loss of around 65.16 million life years due to premature death in the last two years, i.e. 0.0041 life years per person and year (day and a half per person and year). Such number would be lower if the reference was the world’s average life expectancy (72 years), the weighted average of life expectancy according to the number of deaths per country (some 76 years) or the life expectancy of the infected patients, whose frequent underlying pathologies may influence much lower life expectancy without COVID 19 infection. This burden of disease is higher in the countries with the highest reported death rate per COVID-19. Peru, with the highest rate – 6,200 deaths per million inhabitants- would have a burden of disease of around annual 0.0124 life years per person (about 4.5 days per person per year). The burden of disease also varies according to age, with some100 times less in those under 60 (90 % of the world’s population and less than 10 % of COVID-19 deaths). While the long-term impact on disability is still poorly known, its impact on the burden of disease may be counterbalanced by the very controversial lower weight of life years in older age and, in any case, the disability of a high proportion of COVID-19 deaths in patients with co-morbidity due to other causes and thus already a baseline degree of disability. Compared to the overall burden of disease (some 1,706 million-life years due to premature death)[12] COVID-19 caused on average 1.9 % of the overall burden of disease in the last two years. In relation to the most important causes of loss of life years due to premature death, the following list shows the proportion that COVID-19 accounts for each of the causes, according to the diagnostics with COVID-19 and the estimated direct deaths by COVID-19 (60 % of the latter)[13].
Table 1: Overall loss of life years due to pandemic related to other diseases
| Cause | YLLs (000s) | COVID-19 as% of top channels | Estimated 60 % due to COVID-19 |
| All Causes | 1706631 | 1.91 % | 1.14 % |
| Neonatal conditions | 183207 | 17.79 % | 10.68 % |
| Ischaemic heart disease | 175605 | 18.56 % | 11.13 % |
| Stroke | 122115 | 26.69 % | 16.01 % |
| Lower respiratory infections | 105006 | 31.03 % | 18.62 % |
| Diarrhoeal diseases | 68394 | 47.65 % | 28.59 % |
| Road injury | 62279 | 52.33 % | 31.40 % |
| Tuberculosis | 61751 | 52.77 % | 31.67 % |
| Chronic obstructive Pulmonary dis. | 54573 | 59.71 % | 35.84 % |
| Congenital anomalies | 45199 | 72.10 % | 43.26 % |
| Cirrhosis of the liver | 42111 | 77.39 % | 46.43 % |
| Trachea, bronchus, lung cancers | 40849 | 79.78 % | 47.87 % |
| HIV/AIDS | 36131 | 90.19 % | 54.12 % |
| Diabetes mellitus: | 34171 | 95.37 % | 57.23 % |
| COVID-19 | 32588 | 100.00 % | 60.00 % |
| Kidney diseases | 32023 | 101.76 % | 61.07 % |
| Self-harm | 30937 | 105.34 % | 63.20 % |
| Malaria | 30855 | 105.62 % | 63.38 % |
| Interpersonal violence | 25699 | 126.80 % | 76.08 % |
| Colon and rectum cancers | 20570 | 158.42 % | 95.06 % |
| Hypertensive heart disease | 20482 | 159.10 % | 95.46 % |
| Stomach cancer | 19893 | 163.81 % | 98.30 % |
Compared to the loss of life years due to risk factors, the table below shows that the burden of COVID-19 disease is lower than that of the top 7 risk factors. It is striking and worrying to see that the risk factors that lead to much higher loss of human life than COVID 19 trigger far lower investments in research and public health interventions. On the contrary, for many of those risk factors, the private sector invests in marketing much higher than the public health authorities does in prevention of unhealthy life styles based on processed foods high in sugar and salt, tobacco – including second-hand tobacco -, air pollution, interruption of breastfeeding and hyper-medication. Those risk factors lead to obesity, glucose intolerance and hypertension, the main risk factors associated with COVID 19 mortality. Among the causes of highest loss of human life are also those related to global inequities such as malnutrition, lack of access to safe water and sanitation or the shortage of iron and vitamin A. The lockdown measures imposed to control the pandemic by COVID-19 may have significantly increased the loss of life years due to sedentary lifestyles and increased international and subnational inequity. It is unclear whether the control measures have been responsible for less or more life years lost than the virus would have caused itself. Interestingly, as the main mechanism of severe disease and death in COVID-19 infections is the severe inflammatory response (“cytokines’ storm”) it remains to be seen whether the social response causing greater damage than the pandemic itself.
There is a link between the burden of disease in life years operated by COVID-19’s premature death and the other causes globally
Table 2: Overall loss of life years due to pandemic for the main risk factors
| Cause | YLLs (000s) | COVID-19 as% of top channels | Estimated 60 % due to COVID-19 |
| High -lic blood pressure — | 217963088 | 14.95 % | 8.97 % |
| Smoking — | 182478302 | 17.86 % | 10.71 % |
| High fasting plasma glucose — | 170573442 | 19.10 % | 11.46 % |
| High body-mass index — | 147694484 | 22.06 % | 13.25 % |
| Air pollution — | 147418240 | 22.11 % | 13.26 % |
| Child wasting — | 90994816 | 35.81 % | 21.50 % |
| Environment particulate matter pollution — | 83047567 | 39.24 % | 23.55 % |
| Diet high in sodium — | 70398895 | 46.29 % | 27.78 % |
| Diet low in fruits — | 64806281 | 50.29 % | 30.17 % |
| Unsafe water source — | 63892348 | 51.00 % | 30.60 % |
| Household air pollution from solid fuels — | 59472096 | 54.80 % | 32.88 % |
| Drug use — | 41658227 | 78.23 % | 46.94 % |
| Unsafe health — | 41474867 | 78.57 % | 47.15 % |
| Secondhand smoke — | 36316502 | 89.73 % | 53.84 % |
| Diet low in vegetable— | 34210780 | 95.26 % | 57.15 % |
| Iron deficiency — | 33661690 | 96.81 % | 58.08 % |
| Vitamin A deficit — | 28992388 | 112.40 % | 67.44 % |
| LOW physical activity — | 23655862 | 137.76 % | 82.65 % |
| Child stunting — | 19406872 | 167.92 % | 100.76 % |
| Non-exclusive breastfeeding — | 14248898 | 228.71 % | 137.22 % |
The following table summarises the above indicators of magnitude of the pandemic by official data (reported by countries and WHO) and the estimates by population studies and in-depth analysis of cases described above:
Table 3: Measures of the magnitude of the COVID19 pandemic: Official vs estimate data
| cumulative impact | annual mortality | Fatality3 | Annual Sickness Load (FMC)4 | |
| official data | 323000000 | 2770000 | 1.72 % | |
| estimates | 16150000001 | 16620002 | 0.33 % | 33240000
(1.1-1.9 % of the total) |
1: Estimates by multiplying the reported incidence rate by the weighted average incidence ratio of population sero-prevalence studies/official case reports. 2: The average annual mortality attributed to COVID-19 is multiplied by the proportion of deaths seen in autopsy series as directly caused by COVID-19 (60 %) 3: This is the ratio between deaths and incidence. 4: Here only estimated for life years lost because of premature death: Number of deaths due to the difference between the maximum life expectancy and the average death age during the pandemic.
Analysis of the anti-pandemic measures
Any public health intervention (prevention, treatment and rehabilitation) is decided in relation to others (given the resources always limited) according to risk/benefit (harm vs. good), cost-utility ( cost of intervention in relation to the prevention or recovery of healthy life years that would be lost without such action) and opportunity-cost ( relation to the impact of other potential interventions with the same level of resources).
The distribution of a health problem, including the effect of the selected interventions, is measured by unfair or preventable inequalities (inequity) through the “burden of health inequity” (excess deaths or loss of healthy life years in relation to feasible and sustainable levels of health for all).
- Risk-benefit: Prevention and treatment measures against COVID-19 have mainly been lockdowns on mobility and contact in the population, vaccination and treatment. There are significant uncertainties in the level of positive impact of each of these measures, especially if disaggregated by age and health conditions, and even more in their negative impact. To study the impact of a public health measure, a population group (cohort) is monitored over time or compared between a population in which (case) the measure is applied and a population with similar demographic and epidemiological characteristics without such intervention (control). As regards lockdown measures, in most cases, they were generalise, regardless of the incidence and case fatality in each age, sex and health baseline condition group (not well known or published, as described above). Hence, it is not easy to analyse the disaggregated positive impact by population groups. On the other hand, the evolution of natural or induced immunity (the latter after 2021) and the pathogenicity of evolving variants of the virus makes it difficult to estimate by cohorts the impact of each preventive measure. When comparing two populations, as countries, with different prevention policies we find the bias of different demographic, socio-economic and epidemiological situations, and even the information systems themselves. For example, the evolution of incidence and mortality following the lockdown measures between countries in Europe (with high lockdowns) and Africa (with low lockdowns or means to do so) does not seem to indicate a benefit in lockdown measures. On the contrary, the comparison between China and the United States or Europe indicates the opposite. As regards the comparison of incidence and mortality risks among persons using or not using different types of masks in open air spaces, is no significant relative risk evidence to claim that they protect against infection or reduce mortality[14]. As regards the adverse effects of these measures, it can be estimated that global lockdowns accounted for at least 3.363 % of global economic contraction. Such economic loss has been highly uneven (see the inequity analysis below), increasing (through the increase of people under the above-mentioned dignity threshold) possibly up to 10 % the burden of health inequity, some 1.6 million deaths per year and some 56 million life years lost, higher than the COVID-19 direct burden of disease. Another risk of lockdown measures lacking enough analysis is the impact of sedentary life styles in physical health[15] and social isolation on the state of mental health, especially of older people and youth. There are worrying reports on the increase in chronic disease morbidity in the elder and anxiety, depression and suicide rates, particularly among young people[16]. The risk-benefit of the lockdown measures is, hence, unknown yet, but there are signs it may have caused more harm than good. On top of this concern, there is an unmeasured and possibly unmeasurable burden of suffering caused by the systematic lockdown and social distancing taken to the extreme: the dimension of loneliness and related anxiety of the very high proportion of COVID 19 deaths who passed away far from their loved ones. In terms of vaccination, efficacy studies are carried out in case control surveys (costly phase III clinical trials mainly by pharmaceutical corporations) which rendered national and WHO pre-qualification through the assessment of clinical, laboratory and manufacturing practices. The nine WHO prequalified vaccines demonstrated a reduction in mortality above 90 % in vaccines based on mRNA channelled through nano-particles (Pfizer, Moderna) and 60-90 % in viral vectors (Astra Zeneca and Jansen) and 60-70% in attenuated virus-based vaccines (Sinopharm, Sinovac)[17]. Only one protein-based vaccine, Novavax, has been WHO pre-qualified but its coverage is still minimal. Other 24 vaccines have been approved by national regulatory agencies and are awaiting approval by the WHO such as the Russian Sputnik (very similar to Astra Zeneca), three Cuban COVID vaccines and Corbevax (based on proteins). Over a hundred vaccine candidates are pending completion of phase III trials. While some vaccines had a time-gap of less than 2 months from national regulatory approval for emergency use to WHO prequalification, others are still to be approved by WHO after over one year. The cost of scientific writing for peer reviewed high impact journals, the dossiers to apply for prequalification and the inspection of sites and products prevents or delays the process when vaccines are developed in low-income countries. Vaccine induced immunity decreases over time and requires revaccination[18]. In addition to the individual benefit of vaccination in reducing mortality, there is a potential benefit in transmission to third persons (externality), if it reduces the viral burden on mucous membranes. This benefit is limited in vaccinated people[19], who continue to carry the virus on mucous membranes with viral loads that have not been statistically proven to be lower than in unvaccinated pre-infected (with natural immunity). There is very little published and socialized information on natural immunity but recent results on cohorts of people infected with COVID-19 demonstrate better[20],[21] and longer duration[22] (by memory cells in bone marrow studies) than induced immunity. The status of pre-infection or presence of IgG antibodies against COVID 19 antigens should therefore be granted equal mobility rights as vaccinated persons. At present pre-infected persons have no rights of mobility, need recent compulsory PCR –ve or their mobility is restricted to six months after infection, in contrast with the mobility rights of vaccinated persons. This discrimination is against recent evidence of protection through natural immunity. On the other side, pre-infected persons do not gain any further protection by COVID vaccines17 hence the state of pre-infection could or should exempt from the need of vaccination and even less any legal enforcement of compulsory vaccination[23]. Some predict that by March 2022, 60 % of the world’s population will have been infected with COVID-19 variant Omicron[24]: Their exemption from vaccination would have a very important social, economic and political impact. As regards the risk of vaccines, there is lack of transparency in pharma vaccine clinical trial dossiers[25]. On the other side, the very short duration of their follow-up before approval disables any mid- or long-term safety assurance. There are reports of serious side-effects and deaths directly linked to vaccination[26] and myocarditis in young[27] people, indicating 0.0000462 deaths (46 per million) per vaccine[28]. These data enable estimates of risk-benefit, even with only one year of evolution after vaccination, and by age groups, given their very different fatality rate as above mentioned, and pose the question on their use in young people and even more in children. Given the short monitoring period, the risk of vaccination in the medium to long term is even more uncertain, in particular by the novel mechanism of mRNA or DNA based vaccines and their potential interaction with the human genetic structure[29]. Fragments of viral mRNA are known to find reverse transcriptase enzymes and integrate into the human genome in the natural infection process, so vaccination with mRNA copies at much higher concentration than a natural infection may potentially mean reverse transcription into DNA and integration into the human genome of germ cells and even haploid gametes, with potential long term reproductive effects. Although this risk has been considered minimal given the volatility of mRNA in blood circulation, the risk of genetic alteration and its long-term effects in relation to oncogenesis (e.g. HBV[30], HCV, papilloma[31])[32], autoimmune or degenerative processes (as recently seen between Epstein Bar virus and multiple sclerosis[33]) cannot be fully excluded. In terms of treatments, statistically significant effect on reducing mortality has been proven in intensive care and ventilation (CPAP[34] and assisted) in cases of respiratory failure and in nirmatrelvir-ritonavir[35] treatment in severe cases (every 12 hours for 5 days) at a cost of about USD 500 per patient[36]. The risk benefit is deemed sufficient to justify such therapies in severe cases.
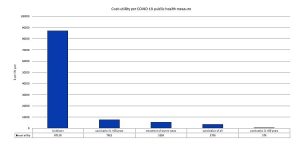
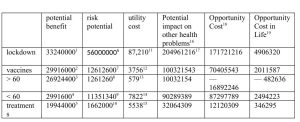
- Cost utility: Utility is measured in life years that an intervention protects (prevents loss) or recovers (by treatment). As mentioned above, there is no absolute evidence of the usefulness of the generalised lockdown measures, as there are no case studies on control and validity of cohorts to demonstrate this, even less disaggregated by age and risk factors, and the uncertainty of risk-benefit for groups with lower risk of COVID-19 related mortality, as discussed above. Even assuming that the lockdown measures could have halved the transmission of the virus and its consequent mortality, the burden of the disease prevented would have been around 32.58 million life years. The global lockdown has caused at least 3.363 % on average annual GDSP[37], or about USD 2.85 trillion. Therefore, the cost utility of the overall lockdown may be around $87,210 per life year potentially lost by COVID-19. Compared to other public health measures, the World Bank and WHO consider relevant interventions of less than $150 per life year in low-income countries and below $500 per ADV in middle-income countries[38]. By comparison, the threshold for utility cost of interventions in the UK public system is $27,400[39] and can reach $100,000 in US private insurance[40], governed by studies of intention to pay by life year. It is striking to see what is the value (or the cost worth investing) of one year of life according to the income levels and the strong correlation with GDP per capita. It is even more telling when we estimate that value to a human life taking into account the world average life expectancy: from some $10,500 in a low-income country to some $ 7 million in high income groups in high income countries. The global lockdown has been most expensive public health intervention in history and at a highest cost per life year, over 5,800 times higher than public health interventions advised by WHO and World Bank in low-income countries. In terms of vaccination, the cost of the available vaccines together with that of distribution by the health system is about $50 per dose. At one dose per six months according to current frequency, the annual cost is around $100 per person. Assuming efficacy rates of 90% in preventing mortality, it could prevent some 29.3 million life years meaning that the of the overall cost utility would be around $26,620 per life year, which is less than the lockdown but still far above the recommended cost utility of public health programmes in middle- and low-income countries. Vaccination of the population over 60 years of age or with risk factors would cost ten times less (as it accounts to 10% of the world’s population) and result in an impact of 90 % of the overall vaccination (as 90% of deaths take place in older than 60 years). Such strategy would also ease the concerns of the risk-benefit considerations described above. The cost utility of vaccination of the population over 60 years of age would therefore be $2,957 per life year. Taking into account the reported benefits of vaccine manufacturing corporations (around $30,000 million for the 12,000 million doses sold), the possible production cost of the vaccines would be around $1.3 per vaccine (sold now at $15-25 per dose). Hence, the cost utility of vaccination over the age of 60 in the world with off-patent vaccines would be $147 per life year, in the affordability range of public health interventions regardless the income levels. In terms of treatment, the cost of entering ICUs and applying mechanical ventilation (CPAP and assisted) during the average 6-day duration, is about 7,500 per patient (in high-income countries the average is $30,000 per admission). Pfizer’s nirmatrelvir-ritonavir is sold at about $500 per treatment course in severe cases. Reducing the mortality if severe cases by 80 % would prevent the loss of some 26 million life years at a cost of about 144,000 million, (10 % of the 160 million cases diagnosed per year x 8 days of average stay in ICUs and treatment of nirmatrelvir-ritonavir). The cost utility of the treatment of severe cases is around $5,538 per life year, beyond the economic reach of low-income or middle-income countries.
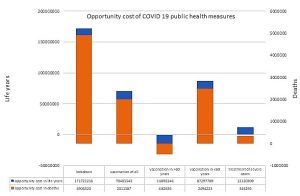
Figure 5: Estimates of cost utility of the measures taken to fight the COVID-19 pandemic in relation to the utility cost thresholds used in countries according to income per capita
- Opportunity Cost: Comparing the cost of COVID-19 control strategies (or loss of economic income) and its impact on the prevention or recovery of healthy life years with those of other public health interventions lacking coverage enables to estimate the cost in life years, and in saved lives, of an excessive cost utility to tackle the COVID-19 pandemic. There are still many prevention and treatment interventions for the main causes of loss of healthy life years (see Table 1: Infectious diseases (diarrhoea, respiratory, malaria, tuberculosis, HIV and HBV) and chronic non-infectious diseases (diabetes, hypertension and its consequences of cardio and cerebrovascular diseases, kidney diseases, lung, colon, prostate and breast cancer),. The average cost utility of those interventions is around $1,000 per life year in low- and middle-income countries. The cost and economic loss of the global lockdown could have, if used in ethical redistribution, reduced almost half of the economic inequity gap above mentioned and prevent around 224 million indirect life years and some 5 million deaths. Regarding vaccination, the full coverage of vaccination would cost some $780,000 million for the protection of some 29.3 million-life years. The selective vaccination coverage of all people over 60 years of age in the world -10 % of the global population –, regardless their nationality and income, would cost some $78,000 million (possibly ten times less deducting the massive profits of corporations) and save some 27.8 million life years. It would also ease the mobility of the youth and, monitored by periodic IgG testing, enable the development of natural immunity and their involvement in social and caring services for the elder, reducing the profound suffering from lonely deaths, as mentioned above. This option is considered highly controversial, but the risk benefit, cost utility opportunity cost and -see below- equity analysis call for age-selective vaccination to be considered. The opportunity cost of vaccinating all under-60 years was above 2.4 million deaths.
Figure 6: Opportunity cost in life years and deaths avoided by decisions of high utility cost vs different COVID 19 measures
The following chart summarises the indicators analysed in relation to the measures taken and currently in force and imposed even through mandatory compliance laws:
1: Estimating that half of the deaths that have occurred may have been prevented by lockdown 2: Estimating 90 % average efficacy of the current available vaccines 3: Taking into account that over 90% of deaths are in people over 60 years old, and that they account for 10 % of the world’s population. 4: Taking into account that < 10 % of deaths are in people under the age of 60, and that they account for 90 % of the world’s population. 5: Taking into account 60 % effectiveness of intensive care treatment in patients with COVID-19 severe disease.. 6: Assuming that the lockdown has increased the overall burden of health inequity by 10 %. 7: By attributing the mortality rate observed in the United States attributed to COVID -19 vaccination. 8: The former applied to the proportion of people over 60 years of age.. 9: The former applied to the proportion of people below 60 years of age... 10: It results from applying 5 % mortality rate due to side effects of ICU treatments in severe cases. 11: Overall economic loss divided by the potential benefit described above. 12: It results from applying the vaccine and distribution system cost of approximately $50 per dose and two doses per year to the entire world population and divided by the potential benefit described above. 13: Idem at 10 %, over the age of 60. 14: Same as 90 % below the age of 60. 15: Same as for severe cases. 16: It results from applying the economic losses of the overall lockdown to equitable economic redistribution and its potential impact. 17: The cost of each intervention is applied to measures with a weighted average utility cost among high-income countries (10 % of the world’s population), a cost utility of $30,000 per life year, middle-income countries (40 %), of 500 $ and low-income countries (50%) of $150. 18: This is the result of subtracting the potential impact on other interventions from the measure itself for COVID-19. 19: It results from estimating preventative deaths by dividing the opportunity cost in life years by the average age of premature deaths (half of the world average life expectancy: 35 years).
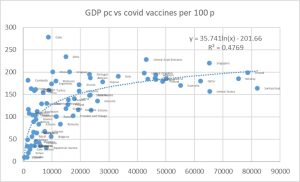
- Equity in public health measures: There is a clear correlation between GDP per capita and COVID-19 vaccination coverage (r2 = 0.4769: Almost half of the change can be explained by GDP per capita). Assuming its effectiveness in reducing morality by 90 % for those infected, the vaccination deficit would have resulted in an unjust and preventable excess of 2,056,462 deaths to date.
Figure 7: Number of COVID 19 vaccines administered per 100 inhabitants vs national average GDP pc
Discussion
While we cannot be sure (partly due to the absence of population seroprevalence studies) of the real COVID-19 incidence (most probably underestimated by official data) or its case fatality (most probably overestimated), available data during 2020 (without vaccination) and 2021 (with availability of vaccines even with high unjust access) point at a loss of around 32,580,000 life years in the world population. This burden is 1.96 % of the loss of life years for all diseases. Moreover, recent studies suggest that direct virus mortality may really be some 60 % of the reported (co-morbidity with positive PCR), so the proportion of the loss of life years due to the pandemic would be lower, some 0.76 % of the total. In relation to the risks that cause the greatest loss of life years, the pandemic has resulted in less than 10 % of the loss of life years due to the effect of either tobacco, agro-industry diets (in both cases with massive marketing funding) or sedentarism, exacerbated by the widespread lockdown measures.
As regards the measures taken against the pandemic at global level and at national and sub-national levels, these have led to an unprecedented cost or economic loss in the history of public health, which deserves consideration without prejudice or ideological, economic or political bias. The studies of efficacy and effectiveness of lockdown and vaccination have not reported results disaggregated by age groups, and by general and COVID-19-specific immunity status and risk factors. On the other side, the short, medium and long-term side-effects of lockdown on physical, mental and social health and indirect health due to economic contraction, as well as those through vaccination, are not entirely known, less so in the medium and long term. The cost utility of the measures taken is of $87,210 per year of life protected by the lockdown, $23,620 for global vaccination and $5,538 for treatment of severe cases. These levels are far above the thresholds of cost utility recommended by the WHO and the World Bank (and the influence of the latter by conditional credits) for low-income ($150 per life year) and middle-income countries ($500 per life year) and even for high income countries regarding vaccination in all age groups. The opportunity cost of lockdown measures in relation to the lack of economic fair redistribution may have resulted in 5.2 million deaths. The opportunity cost of COVID 19 vaccination in all age groups in relation to the lack of coverage of other much more efficient (cost-effective) public health interventions -in particular in low-income countries-, is of over 2 million deaths. The only public health intervention that has no opportunity cost in relation to other global health challenges is the selective vaccination for older than 60 years regardless country or income group.
The impact of the pandemic on global equity suggests that, while there is no higher burden in low-income countries (discriminated against in the right to health as described above), the effects of the economic contraction will most likely increase overall economic inequity and hence inequity in health by some 10%. Besides, inequitable vaccination coverage, biased towards middle-income and high-income countries, has led to an unfair and preventable excess of 2,056,462 deaths in lower-middle-income countries and low-income countries during 2021-2022.
Recommendations
- Global redistribution of economic resources towards global economic equity that can prevent more than 10 million unfair deaths per year.
- Promote healthy lifestyles correlated with sustainable ecological and carbon footprint for new generations and prevent more than 2 million deaths per year due to the effects of climate change in the rest of the century, progressively higher and hitting the least polluting countries harder[41].
- Global equitable financing of a Global Research and Public Goods Fund, outlawing knowledge patents for vital and life-saving knowledge and goods (oxygen, water, food, essential medicines).
- Access to serological tests on a regular basis to identify persons and groups protected by natural immunity, by vaccine-induced protection or non-immune and their risk and responsibility to avoid infecting other persons or loving care for severe patients.
- Comprehensive access to effective and safe vaccines (including the support to the pre-qualification processes for vaccines from low-income countries, as the Cuban protein-based COVID 19 vaccines).
- Global sequential coverage prioritizing non-immune persons over 60 years old and/or with risk factors, rather than the present inequity pattern of income and nationality.
- Assess the pertinence of vaccination in younger age groups in terms of risk/benefit, cost-effectiveness and opportunity in relation to other global health challenges.
This must be based on an open and uncensored, evidence-based debate based on the universal right to health and the ethical principle of equity.
References
[1] For the period 1960-2010 there were 14 countries with constant HRS criteria, for 1960-2015, 7 countries and for the 1960-2020 period only one country.
[2] http://www.peah.it/2021/04/9658/
[3] The region of Ipeiros in Greece has an annual GDP pc below the excess threshold and life expectancy above the best national average, Japan.
[4] Https://www.worldometers.info/coronavirus/coronavirus-age-sex-demographics/
[5] Https://ourworldindata.org/grapher/total-covid-cases-deaths-per-million
[6] Https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7584920/
[7] Https://www.thelancet.com/journals/langlo/article/PIIS2214-109X (20) 30544-1/fulltext.
[8] Https://www.ajtmh.org/view/journals/tpmd/104/6/article-p2176.xml
[9] Https://www.pnas.org/content/118/21/e2105968118
[10] Https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-hospital-activity/
[11] Https://www.who.int/data/gho/indicator-metadata-registry/imr-details/159
[12] Https://www.healthdata.org/gbd/2019
[13] Https://elpais.com/sociedad/2022-01-14/los-datos-de-hospitalizados-con-el-coronavirus-incluyen-hasta-un-40-de-pacientes-ingresados-por-otras-dolencias.html
[14] Https://www.cebm.net/covid-19/masking-lack-of-evidence-with-politics/
[15] Https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8685753/
[16] Https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0255251
[17] Https://www.healthdata.org/covid/covid-19-vaccine-efficacy-summary
[18] Https://www.nejm.org/doi/full/10.1056/nejmoa2114228
[19] Https://www.thelancet.com/journals/laninf/article/PIIS1473-3099 (21) 00690-3/fulltext.
[20] https://www.medrxiv.org/content/10.1101/2021.08.24.21262415v1.full
[21] https://www.cdc.gov/mmwr/volumes/71/wr/mm7104e1.htm
[22] Turner, J.S., Kim, W., Kalaidina, E. et al. SARS-CoV-2 infection induces long-lived bone marrow plasma cells in humans. Nature 2021
[23] Https://www.bmj.com/content/374/bmj.n2101/rr-0
[24] Https://www.healthdata.org/covid/video/insights-ihmes-latest-covid-19-model-run
[25] Https://www.transparency.org/en/press/covid-19-vaccines-lack-of-transparency-trials-secretive-contracts-science-by-press-release-risk-success-of-global-response
[26] Https://www.bmj.com/content/373/bmj.n1372/rr-2
[27] Https://pubmed.ncbi.nlm.nih.gov/34614329/
[28] Https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/adverse-events.html
[29] Https://www.pnas.org/content/118/21/e2105968118
[30] Https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4065878/
[31] Https://www.ncbi.nlm.nih.gov/pmc/articles/PMC523272/
[32] Https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6212953/
[33] Https://www.science.org/doi/10.1126/science.abj8222
[34] Https://pubmed.ncbi.nlm.nih.gov/33889343/
[35] Https://www.pfizer.com/news/press-release/press-release-detail/pfizer-announces-additional-phase-23-study-results
[36] Https://www.precisionvaccinations.com/2021/11/18/pfizers-covid-19-oral-antiviral-cost-529-course
[37] Https://data.worldbank.org/indicator/NY.GDP.MKTP.KD.ZG
[38] Https://pubmed.ncbi.nlm.nih.gov/32812212/
[39] Https://www.gov.uk/guidance/cost-utility-analysis-health-economic-studies
[40] Https://www.sciencedirect.com/science/article/pii/S1098301519301482