Despite designing some targeted programs for financial support for the poor in Iran, many poor people are left out of coverage due to the fragmentation of the programs. But what makes such challenges for a health system to reach the poor? It will be hard to make substantial progress towards pro-poor UHC without promoting simultaneously universal social protection that will contribute to realize SDG 1 targets of alleviating poverty. This requires system-wide social and health policies breaking the boundaries of traditionally fragmented welfare systems and health programs, where there is a "Berlin Wall’ that separated health and social care services. There is a Ministry of Cooperatives, Labor and Welfare (MCLW) in charge of universal health protection and Ministry of Health and Medical Education (MOHME), who is the steward of the universal health coverage and health insurance system, without a clear cooperation line which makes a thick berlin wall among these two files
By Dr. Manal Etemadi
Health financing researcher, Iran Health Insurance Organization (IHIO), Tehran, Iran
The Berlin Wall Between Welfare and Health in Iran: Who Gains the Health Subsidies?
Health financing policies must face the question of how to increase equitable financing, this implies progressive financing which means that the rich pay a greater share of their income than the poor. In many countries, the lowest income deciles experience less catastrophic health expenditure than the highest income deciles which reflects the nature of the patient cost sharing. When people are very poor, they don’t use services so they don’t have to pay and therefore don’t expose to catastrophic expenditure. If their income situation improves, they will begin to use services but will suffer the adverse financial consequences associated with paying for care.
Two main challenges must be considered for improving the equity in health financing: firstly, that families do not become poor or do not pay a large share of their income to receive the necessary health care, and secondly, that poor families pay less than rich families. Poor families not only have less income, but a larger share of their income is spent on basic needs such as food and shelter. Every family should pay a fair share of the health system costs, and when it comes to the poor, a fair share may mean not paying.
Due to the increase in demand towards the private sector for interventions that are not included in the basic benefit package, the impact of out-of-pocket payments on the poor must be considered. One of the four main determinants of the financing performance of a health system is the flow of subsidies to the poor. Cost sharing mechanisms reduce the demand for services totally and harms the poor. Even when services are free, they are not necessarily affordable for the poor because other costs associated with seeking health care, such as the cost of medicines, informal cost to providers, transportation, and time lost to work, are also important. Even when there are exemptions or subsidies to cover the costs of the poor, other factors prevent the poor from using health services that are difficult to assess: the reluctance of the poor to seek services due to stigma or the way health workers treat them.
The financing strategy should ensure that the poor receive the service they want in time of illness without financial barriers. Therefore, out-of-pocket payments for care, especially for the poor, should not be considered a long-term source of health system financing.
Public spending on basic services, i.e., primary health care, benefits the poor, while the main beneficiaries of subsidies for tertiary hospital are the non-poor. The poor rely more on public health care facilities, while wealthier families use private hospitals and private care services. The lower costs of public health compared to hospitals tend to support the poor, while hospital costs and the provision of drugs are not well targeted. Hospitals and infrastructure costs are not pro-poor and progressive. Evidence also shows that spending on infrastructure disproportionately benefits the non-poor. The most effective way to improve the health system for the poor is to identify their most urgent health needs of the poor and design an effective way to meet those. Focusing on the specific needs of the poor may not save money, but it does ensure that what is spent is well targeted.
In order to realize the purpose of targeting, which includes minimizing the leakage of benefits to non-target groups in order to maximize the resources available for targeting the desired group, the inclusion error (or leakage error which means the proportion of non-target people who benefit from the benefits of the intervention) and the exclusion error(or coverage error which means the ratio of people from the target group who do not benefit from the benefits of the intervention) should be distinguished and balanced in policy formulation.
To direct more health benefits to the poor, since the poor are less likely to use services than the rich, public health programs may use targeted strategies. The application of targeted mechanism in insurance system which includes high subsidization, integration of subsidized people and participating people, balanced benefits package for all and reduced cost sharing, are considered as effective measures to expand insurance coverage for poor people. Targeting strategies may identify the poor as eligible for specific benefits, implement programs in specific areas where the poor live (as has been stipulated in general health policies in Iranian health system), or cover health problems that the poor often experience. Programs that use multiple targeting approaches will be more effective. In addition, where governments define a cost sharing for public health services, waiver strategies and Sliding – scale fees will be critical to successfully direct benefits to the poor.
As the very poor cannot afford to pay for health services, governments must guarantee the financing of health services for them, and especially for the use of hospital care, either through direct payments from tax revenues or through cross-subsidies in health insurance-based systems. Political pressures may prevent changes in the allocation of resources to the poor, and limited government capacity may prevent the effective implementation of exemption programs to protect the poor, what we can see in Iranian health system. In allocating public resources, policymakers should give priority to public health and disease prevention and subsidies for the poor.
Iran, as a populated lower-middle income country which suffered from severe financial constraints and limitation due to economic sanctions, already struggled with health financing. There is a Two-tier health system with private sector’ which served better-off and some of the poor obliged to refer only to public sector and also a tiered health insurance system with inequitable benefit packages for different segments of the population, including complementary and supplementary health insurance only for the better-off that the poor don’t have the access to it. There is separated delivery system for most of the poor through family physician and referral system. Despite the fact that the law requires the health system to design the cost-sharing based on the income levels, all the poor have to pay same rate of user fee at the point of service delivery, except the rich who enjoyed the complementary health insurance and in most cases they don’t have to pay considerable fee from the pocket at the point they receive their needed services.
What is considered in Iran in the form of specific and official programs for financial protection for the poor is divided into two main parts: Health insurance programs include subsidized insurance coverage for poor people and the non-insurance programs include providing low-cost services to all in public hospitals and unstructured cost-sharing reduction for poor people in public hospitals in the case that the poor claim they are not able to pay the cost of services, which has led to outpatient services and especially Medicine still has a high out-of-pocket payment burden. Supply-side subsidies in the form of low cost of all services for all patients in public hospitals, benefit the rich more than the poor, as the Inverse Care Law which claims that the poor bear the greatest burden of disease, but have a smaller share of health care, and thus the public subsidized services (from the simplest to the most complex and expensive services provided in public hospitals) are mostly benefit the rich than the poor, who are the main target group of these services. This is because due to the lower price of services in the public sector, any use of the services by people with higher incomes is a subsidy for this group.
Despite designing some targeted programs for financial support for the poor in Iran, many poor people are left out of coverage due to the fragmentation of the programs. But what makes such challenges for a health system to reach the poor? It will be hard to make substantial progress towards pro-poor UHC without promoting simultaneously universal social protection that will contribute to realize SDG 1 targets of alleviating poverty. This requires system-wide social and health policies breaking the boundaries of traditionally fragmented welfare systems and health programs, where there is a “Berlin Wall’ that separated health and social care services. There is a Ministry of Cooperatives, Labor and Welfare (MCLW) in charge of universal health protection and Ministry of Health and Medical Education (MOHME), who is the steward of the universal health coverage and health insurance system, without a clear cooperation line which makes a thick berlin wall among these two files.
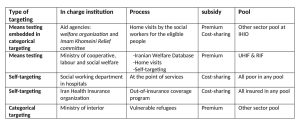
In insurance programs in Iran, where the government takes the place of the employer and provides subsidized coverage, it is not able to protect people equally from catastrophic health expenditure, and previous plans in Iran Health Insurance Organization, as the main public health insurer in Iran, including urban hospitalization insurance and the Rural health insurance program have had regressive effects on the distribution of health care financing as ignored the progressive factor of financing. Urban Hospitalization Insurance, which was designed in 2002 with the aim of covering uninsured people in cities and became known as urban vulnerable people insurance, is an example of non-targeted subsidized insurance in the country, which was literally changed to the self-fund pool (Iranian Pool) and was continued with a discount in the payment of insurance premiums for the poor. In the Universal Health Insurance Pool and Rural Health Insurance Pool, without distinguishing the poor from the rich, this subsidy is allocated for insurance premiums, and this issue causes to waste earmarked resources toward the rich. Table 1 indicated some programs designed to protect the poor in health system of Iran.
Targeting mechanisms for social health assistance
In formulating financial support policies for the poor in Iran, type 1 error in policy making leakage error, is considered the main policy tool. Policy makers are not willing or believe (or both) to target the health subsidies and therefore the resources are earmarked for the poor which the rich people benefit more. Therefore, due to the imposition of a heavy cost burden and beyond the capacity of the determined resources with the entry of the rich into the plan, designed policy has failed, been redesigned, and usually become limited. The current policies to support the poor have design benefits to the poor that the majority of the poor population do not have correct and complete information about them, do not have the correct referrals to receive support, and sometimes espose to higher costs and pay higher out of their pocket.
The health system in Iran has not been able to make effective interventions in financial support for the health of the poor. Moving the supply side subsidies to the demand side in health insurance system in the form of exemption policies for the identified poor in the comprehensive social protection system is the first step to targeting the subsidies to the poor.
Generally, in countries with a similar socio-economic situation to Iran, there is a need for targeted policies for the poor in the economic and health sectors in parallel, and reducing poverty while ensuring the poor have financial access to health services should be followed up together. By designing targeted programs for the poor including focusing on their specific diseases and conditions, calculating and reducing the burden of out-of-pocket payments for all health services, especially the services that the poor use the most and exemption from paying for them, increasing the health literacy of the poor, improving the social determinants of health in the places where the poor live, to name but a few, can prevent the poor from falling into the poverty trap and becoming poorer because of treatment costs and should be on the agenda of the government. Focusing on targeted programs to financially support the poor is a necessary prescription for Iran because evidence has shown that untargeted programs leave the poor behind.
References
- WHO. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies: World Health Organization; 2010.
- Murray CJ, Frenk J. A framework for assessing the performance of health systems. Bulletin of the world Health Organization. 2000;78(6):717-31.
- WHO. The world health report 2000: health systems: improving performance: World Health Organization; 2000.
- Etemadi M, Hajizadeh M. User fee removal for the poor: a qualitative study to explore policies for social health assistance in Iran. BMC Health Services Research. 2022;22(1):1-12.
- Gafar J. Do the poor benefit from public spending? A look at the evidence. The Pakistan Development Review. 2005:81-104.
- Fogel RW, Lee C. Who gets health care? National Bureau of Economic Research, 2003.
- Jacobs B, Price A. A comparative study of the effectiveness of pre-identification and passive identification for hospital fee waivers at a rural Cambodian hospital. Health and social protection: experiences from Cambodia, China and Lao PDF. 2008.
- Mathauer I, editor State budget subsidization of poor and vulnerable population groups in health insurance type schemes in low-and middle-income countries: A global overview and trends in institutional design. Bangkok: Prince Mahidol Award Conference; 2015.
- Ashford LS, Gwatkin DR, Yazbeck AS. Designing health and population programs to reach the poor. 2006.
- Bennett S, Gilson L. Health financing: Designing and implementing pro-poor policies. 2001.
- Heller MPS. What Should Macroeconomists Know about Health Care Policy?: International Monetary Fund; 2007.
- WHO. The world health report: health systems financing: the path to universal coverage2010.
- Maher A. The relationship between poverty and health in Iran. Journal of Social Welfare. 2005;5(18):1-19.
- Moradi-Lakeh M, Vosoogh-Moghaddam A. Health sector evolution plan in Iran; Equity and sustainability concerns. International Journal of Health Policy and Management. 2015;4(10):637-40.