IN A NUTSHELL
Author's note
 …This article draws from my work in health governance and medico-legal practice and illustrates, through real cases across Africa, why legal literacy deserves greater attention within health systems. It highlights how a stronger understanding of human rights, administrative justice, informed consent, and proper documentation can prevent harm, strengthen accountability, and ultimately support the goals of UHC…
…This article draws from my work in health governance and medico-legal practice and illustrates, through real cases across Africa, why legal literacy deserves greater attention within health systems. It highlights how a stronger understanding of human rights, administrative justice, informed consent, and proper documentation can prevent harm, strengthen accountability, and ultimately support the goals of UHC…

By Sylvia Penelao Hamata
Nurse | Midwife | Lawyer |
President, Independent Midwives Association of Namibia (IMANA)
Legal Literacy: The Missing Pillar In Universal Health Coverage
INTRODUCTION
Universal Health Coverage (UHC) is not only about providing services and financial protection, but also about ensuring quality care, accountability, and the protection of patients’ rights. Legal literacy – the understanding of laws, rights, and duties in healthcare – is a crucial yet often overlooked pillar of UHC. When healthcare workers and policymakers lack awareness of legal obligations (such as informed consent, proper documentation, non-discrimination, and administrative justice), the consequences can be tragic for patients and costly for governments. Below, we examine landmark hospital negligence and health rights cases from across Africa (Southern, West, and East Africa) that illustrate how gaps in legal literacy led to harm, and how strengthening legal understanding in health systems could prevent such incidents. Each case underlines that empowering health professionals with legal knowledge helps protect patient rights, reduce harm, and reinforce accountability – thereby strengthening UHC.
LANDMARK CASES
Namibia: Theonistar /Naris – Post-Operative Negligence and Accountability
Background & Outcome: In April 2018, 11-year-old Theonistar /Naris underwent a routine tonsillectomy at a rural Namibian hospital (Khorixas State Hospital). Post-operative complications arose – specifically excessive bleeding – and over the next few days Theonistar’s condition deteriorated until she died on April 14, 2018 org.na. Her parents sued Namibia’s Ministry of Health and Social Services, alleging that the doctors and staff were negligent in monitoring and managing the bleeding. The case drew national attention as an emblematic failure of patient safety. In September 2024, the lawsuit concluded with a court-approved settlement, bringing a measure of closure for the family lac.org.na. The settlement implicitly acknowledged shortcomings in care and underscored the legal consequences of such medical failures in Namibia’s health system lac.org.na. Observers noted that this tragic case shone a spotlight on systemic challenges – like understaffing, poor post-operative surveillance, and slow emergency response – that must be addressed to prevent future harm lac.org.na.
Preventable Through Legal Literacy: This case illustrates how improving healthcare workers’ legal literacy could have averted a preventable death. If the surgical and nursing team had been more aware of their duty of care and legal accountability, they might have adhered more vigilantly to post-op monitoring protocols and escalated care at the first sign of hemorrhage. Better understanding of patient rights and safety standards – for example, recognizing that failing to respond to clear signs of distress violates the patient’s right to life and health – could have prompted staff to seek timely surgical re-intervention or transfer to a higher-level facility. In addition, solid knowledge of documentation practices might have ensured that Theonistar’s post-operative vital signs and complaints were properly charted and communicated, allowing senior clinicians to intervene earlier. In short, had the providers treated the situation not just as a clinical routine but as a matter of legal and ethical obligation, Theonistar’s worsening bleed may have been addressed before it turned fatal.
Avoidable Litigation and Reputational Costs: The absence of legal foresight ended up costing the Namibian authorities. The government had to engage in a protracted legal battle from 2018 to 2024, diverting resources to defend the case and ultimately agreeing to a financial settlement for the family. Beyond monetary costs, the Ministry of Health suffered reputational damage as the case became public. Media coverage and a national debate highlighted “the potential legal consequences of medical failures,” putting pressure on the health system to reform org.na. In a country striving for UHC, such highly publicized negligence erodes public trust in health services. That loss of trust is itself a setback for UHC goals, as patients may avoid seeking care if they fear negligence. Investing in legal literacy – training health workers to understand and respect legal standards – is far cheaper and better for public confidence than defending negligence cases or paying out settlements for avoidable tragedies.
Policy and Training Gaps Exposed: The Theonistar /Naris case exposed gaps in policy and training at the hospital and national level. Notably, it revealed insufficient training in post-operative emergency care for rural hospital staff and a lack of clear protocols to ensure accountability for monitoring patients. It also pointed to an absence of routine legal-risk awareness: frontline providers appeared unaware that inadequate care could breach legal standards (such as the standard of care expected, or even potentially the constitutional right to health). This suggests a need for policies that require regular training on patient safety and rights. As Namibia’s Legal Assistance Centre noted, the case “underscores the need for reforms in medical practice and procedures, especially in rural hospitals” org.na. Ensuring that healthcare workers know the medicolegal implications of negligence – and that they can be held accountable in court – can create a culture of greater diligence. Following the case, stakeholders have called for improved clinical governance, better supervision and mentoring in district hospitals, and integrating human-rights principles into medical education. These steps would treat legal literacy as a core competency, ultimately preventing harm and reinforcing accountability in pursuit of UHC.
Namibia: LM and Others v Government – Coerced Sterilisation of HIV-Positive Women
Background & Outcome: This landmark Namibian case involved three women (identified pseudonymously as LM and Others) who were subjected to sterilisation procedures in public hospitals without their informed consent. All three women were HIV-positive mothers who, after delivering babies via caesarean section, later discovered that doctors had permanently sterilized them (by tubal ligation) without properly explaining the procedure or obtaining voluntary consent law.harvard.edu. The women sued the Government of Namibia, arguing that this practice was a gross violation of their rights to bodily integrity, health, and family. In 2012, the High Court of Namibia ruled in the women’s favor, finding that the sterilizations were indeed carried out without informed consent and thus unlawful humanrightsclinic.law.harvard.edu. The court held that merely having a signed consent form was not sufficient if genuine understanding and voluntariness were absent. The Government appealed, but in 2014 Namibia’s Supreme Court affirmed the verdict: sterilization without full, informed consent is a violation of constitutional rights humanrightsclinic.law.harvard.edulaw.cornell.edu. While the Supreme Court did not find definitive proof of intentional discrimination against the women based on HIV status (as the plaintiffs alleged), it unequivocally condemned the lack of informed consent in these procedures law.cornell.edulaw.cornell.edu. The ruling was celebrated as a victory for women’s rights – confirming that patients’ reproductive choices must be respected and that paternalistic medical practices have no place in modern healthcare law.cornell.edu.
Preventable Through Legal Literacy: The LM case vividly demonstrates how improved legal literacy among healthcare providers could have prevented harm and rights abuses. Informed consent is both an ethical cornerstone and a legal requirement for any surgical procedure – especially one as life-altering as sterilization. Had the doctors and nurses involved been adequately trained in the law of consent and patients’ rights, they would have understood that pressuring a woman in labor to sign a consent form, or obtaining consent through incomplete information, is not legally valid. Indeed, the Supreme Court emphasized that a decision as personal as sterilization “must be made with informed consent, as opposed to merely written consent ”cornell.edu, and that there is no place for “medical paternalism” in deciding such matters law.cornell.edu. With stronger awareness of this principle, healthcare workers would have ensured the women were counseled thoroughly about the procedure’s permanent consequences, given the option to defer the decision, and free from coercion – or simply not sterilized them at all without explicit request. Furthermore, legal literacy training could have highlighted the human rights implications and potential liabilities of coerced sterilisation. The providers might have been deterred from their actions had they known that violating patients’ reproductive rights could lead to courtroom scrutiny and judgments against them. In essence, instilling knowledge about patients’ autonomy, dignity, and the legal mandate of consent would likely have averted this violation of rights.
Avoidable Litigation and Reputational Costs: The fallout of this case showed how costly ignorance of the law can be for governments. The Namibian government spent several years in court, from the initial 2012 lawsuit through a Supreme Court appeal in 2014, defending an indefensible practice. Besides the direct legal costs and the prospect of paying compensation to the women, there was significant reputational damage. International and domestic observers decried the coercive sterilisation of HIV-positive women – a practice described as “a wrongful and unlawful” violation of rights orghumanrightsclinic.law.harvard.edu. The case tarnished the public image of Namibia’s health services, potentially deterring some women (particularly those living with HIV) from seeking care out of fear of mistreatment. This is directly counter to UHC goals, which require that everyone – including marginalized groups – trust the health system enough to use it. Government officials also had to contend with public protests and campaigns led by civil society (like the Namibian Women’s Health Network and Southern Africa Litigation Centre) pushing for redress humanrightsclinic.law.harvard.eduhumanrightsclinic.law.harvard.edu. All these impacts could have been avoided or mitigated with better legal compliance upfront. By educating healthcare workers on patients’ legal rights and by enforcing consent policies in hospitals, the state could have prevented the abuses instead of reacting to them. In hindsight, the case underlines that proactive legal literacy is far less costly than reactive litigation – both in fiscal terms and in maintaining public confidence in the health system.
Policy and Training Gaps Exposed: The LM v Namibia case revealed critical gaps in health system policy and training at the time. At a policy level, it became clear that hospital consent protocols were deficient – there were no safeguards to ensure that consent for procedures like sterilisation was truly informed and freely given (for example, no policy requiring an independent counselor or a waiting period for sterilization consent). This gap allowed individual providers’ biases (such as stigma against women with HIV having more children) to translate into irreversible harm. On the training front, the case highlighted a lack of rights-based training for health workers: staff were evidently not sensitized to the reproductive rights of patients or the legal and ethical standards for obtaining consent. Documentation practices were also poor – the fact that signed forms existed gave a false sense of security, whereas proper procedure would require detailed documentation of counseling and voluntary consent. Following the court rulings, there have been calls in Namibia and across the region for better integration of human rights education in medical and nursing curricula law.harvard.edulaw.cornell.edu. Policies have since been advocated (and in some cases implemented) to ensure that no woman can be sterilized without a robust consent process free from duress – for instance, mandating that consent for sterilisation must be reaffirmed postpartum (when the patient is no longer in pain or under stress). The case’s legacy is a push for health systems to treat legal literacy as a necessity: clear guidelines, continuous training on informed consent and anti-discrimination, and accountability measures so that the rights of patients are upheld as part of delivering universal healthcare.
Ghana: Helena Nyamekye – Maternal Death and Negligence in Childbirth
Background & Outcome: In Ghana, a high-profile medical negligence case underscored the importance of respecting patient choices and adhering to standards of care during childbirth. Mrs. Helena Brema Nyamekye, a 27-year-old woman (and PhD student), died in November 2015 at Accra’s 37 Military Hospital due to complications in labor. The tragedy unfolded after Helena – who had a history of high blood pressure – requested a caesarean section (C-section) when she was due to deliver, knowing her condition put her at risk org.gharhr.org.gh. The doctors, however, denied her request and insisted on attempting a normal vaginal delivery, without providing a credible medical reason for refusing the C-section arhr.org.ghmyjoyonline.com. During labor, Helena suffered profuse bleeding and other complications; she was eventually taken to an operating theatre, but by then it was too late – she hemorrhaged to death after delivery arhr.org.gharhr.org.gh. Her newborn baby was left with a permanent injury to his arm, and her husband (a retired military officer) and father sued the hospital and the Attorney General for negligence. In July 2021, the Accra High Court ruled in the family’s favor, finding 37 Military Hospital liable for the negligence of its staff that led to Helena’s preventable death arhr.org.gharhr.org.gh. The court was unequivocal that Helena’s death “was a preventable one”, caused by the failure of the hospital to act on her condition and requests arhr.org.gh. Justice Kwaku Ackaah-Boafo, in a strongly worded judgment, noted that no plausible explanation was given by the doctors as to why Helena’s C-section request – made hours before delivery – was not honored myjoyonline.commyjoyonline.com. He also observed that during her labor, no doctor or house officer was present to monitor her, reflecting a lapse in basic care arhr.org.gharhr.org.gh. The court awarded over GH¢1,000,000 (around US$170,000) in damages to the family – including compensation to Helena’s husband and father for the lost life, and to her infant son for his injury and suffering arhr.org.gharhr.org.gh. This was one of the heaviest negligence judgments in Ghana’s recent history, sending a clear message about accountability in maternal healthcare.
Preventable Through Legal Literacy: The Helena Nyamekye case highlights how greater legal and rights literacy among health professionals could have prevented a maternal fatality. Firstly, informed consent and patient autonomy were glaringly disregarded – Helena’s express wish for a C-section was overridden by providers who “should have known what was best” but failed to justify their decision org.gh. If those providers had been trained to respect patients’ rights and choices (a key legal and ethical tenet), they would have either honored her request or engaged in a thorough informed consent process discussing the risks and options. Legally literate healthcare workers would recognize that a patient has the right to refuse or request certain treatment and that ignoring her could constitute a breach of duty. Secondly, awareness of standards of care and duty of care from a legal perspective would have alerted staff that proceeding with a high-risk normal delivery (especially in a hypertensive patient) without proper monitoring could be deemed negligent. For instance, a legally-aware obstetric team would know that failing to have any doctor present during labor, or not utilizing available blood supplies during hemorrhage, could violate the standard of care and thus expose them to liability arhr.org.gharhr.org.gh. Basic legal literacy in this context means understanding that every reasonable precaution (like honoring a reasonable request for C-section, or at least continuous monitoring) must be taken to safeguard the patient’s life. Had the hospital personnel internalized this, they likely would have acted more urgently and cautiously, treating Helena’s case not as just another delivery but as one where they were accountable for preventing harm. Ultimately, training in human rights and equity might also have made a difference: if the staff viewed the situation through a rights lens, they would have seen Helena as entitled to the best possible care (especially as her condition was life-threatening), rather than subject to the convenience or judgment of the providers. In summary, infusing legal literacy – understanding consent laws, negligence standards, and patients’ rights – into obstetric practice could have saved Helena’s life.
Avoidable Litigation and Reputational Costs: The consequences of this negligence were dire not only for the family but also for the government and health system. The financial award of GH¢1.075 million is a significant cost to a public hospital – funds that could have been used for improving maternity wards or training staff were instead paid out due to a preventable error org.gh. The litigation process itself (spanning several years from the 2015 incident to the 2021 judgment) consumed judicial resources and cast the health facility in a negative light. The case was widely reported, with headlines about the court “slapping” the hospital with damages for a maternal death arhr.org.gh. This publicity undoubtedly eroded public trust in one of Ghana’s major hospitals. Women reading about the case might fear that their preferences in childbirth will be ignored or that they could face similar neglect – a fear that can discourage utilization of maternal health services. Such reputational damage strikes at the heart of UHC: if people do not trust the quality and responsiveness of care, universal access on paper will not translate to actual use of services. By contrast, had the hospital demonstrated a culture of accountability and respect, the tragedy – and ensuing backlash – could have been avoided. The case has since spurred calls for better training of healthcare providers on medical negligence and patient rights myjoyonline.com. Indeed, the Ghana Health Service and professional associations have been urged to incorporate legal issues into continuing education – emphasizing that compassionate, patient-centered care is not just ethical but also essential to avoid legal liability. In the long run, strengthening legal literacy and accountability mechanisms is a far more reputationally positive strategy for health authorities than defending negligence claims in court.
Policy and Training Gaps Exposed: The court’s findings in the Helena Nyamekye case pinpointed several systemic gaps. A major gap was in clinical governance and oversight: the fact that no doctor was present or on call during a high-risk labor indicates a policy failure in staffing and supervision org.gh. This suggests the need for clear protocols ensuring that complex deliveries (especially when a patient has hypertension or requests a surgical delivery) are attended by appropriately senior clinicians. The case also exposed a training gap in obstetric emergency management – for example, the team did not formulate a proper plan to monitor and respond to Helena’s hemorrhage, nor did they utilize available blood transfusion timely arhr.org.gh. Such lapses point to insufficient drills or guidance on handling obstetric hemorrhage, which is a leading cause of maternal death. Importantly, the judgment lamented the “lack of attention” in patient care and urged health workers to be “extra professional” arhr.org.gh, hinting at the need for a mindset shift via training. Incorporating modules on medical law and ethics into training can reinforce why protocols must be followed – not only for clinical reasons but because the law demands due diligence and fairness in treatment. Additionally, the hospital’s reluctance to honor the patient’s choice of C-section reflects a policy gap regarding informed consent and birth choices. Policies may need updating to explicitly require that maternal requests (when medically reasonable) are given serious weight, and any refusal of such a request be justified in writing. In sum, this case advocates for policy reforms such as: regular audits of maternity care quality, mandatory training on patients’ legal rights, and establishing a complaints mechanism whereby patients’ concerns (like a request for a different mode of delivery) are heard and documented. By addressing these gaps, Ghana’s health system can move closer to a UHC model that guarantees not just access, but respect and safety for patients.
Nigeria: Dr. Orji – Criminal Liability for Medical Negligence
Background & Outcome: In an unprecedented case in Nigeria, a doctor was criminally convicted and sentenced to imprisonment due to reckless treatment of a patient – underlining that severe medical negligence can attract personal liability. Dr. Ferdinand Ejike Orji, the Medical Director of a private facility (Excel Medical Centre in Lagos), treated a 16-year-old boy who had sustained a fracture in his left leg com. The boy, a talented basketball player, had returned from the United States for holidays when he broke his leg, and he was brought to Dr. Orji’s clinic for care thisdaylive.com. Despite not being an orthopaedic specialist, Dr. Orji proceeded to handle the case in a grossly substandard manner. He applied a plaster-of-paris (POP) cast on the broken leg without first conducting an X-ray to properly assess the fracture thisdaylive.com. Worse, the cast was applied by personnel who were not qualified, and Dr. Orji did not obtain informed consent from the boy’s mother for this treatment thisdaylive.com. After the cast was applied, the patient experienced severe pain and swelling – classic signs of compartment syndrome, a limb-threatening complication. Shockingly, Dr. Orji willfully refused to remove or loosen the cast despite the escalating pain, leaving the condition to worsen thisdaylive.com. By the time the boy was finally taken elsewhere, the damage was done: the unrelieved compartment syndrome permanently damaged his leg, ending his hopes of a sports career thisdaylive.com. The Lagos State authorities filed criminal charges against Dr. Orji, accusing him of recklessly endangering the patient’s life and causing grievous harm. In January 2023, the Lagos High Court found Dr. Orji guilty on four counts of negligence and breach of duty, noting that his conduct fell far below the expected standard for a medical practitioner thisdaylive.comthisdaylive.com. The court held that his actions – especially ignoring the mother’s lack of consent and the patient’s pleas – amounted to criminal negligence. He was sentenced to one year in prison on each count (to run concurrently) thisdaylive.comthisdaylive.com. This judgment, now under appeal, is considered a landmark in Nigerian medico-legal jurisprudence as it signaled a readiness to impose penal consequences on healthcare workers for egregious malpractice thisdaylive.comthisdaylive.com. It sent shockwaves through the medical community, reinforcing that patient safety is not just a civil matter but can engage criminal law when recklessly disregarded.
Preventable Through Legal Literacy: The Dr. Orji case is a dramatic example of how a stronger foundation in legal and ethical standards could have prevented harm to the patient and kept the doctor out of jail. Key failings in this case – treating outside one’s competency, lack of informed consent, ignoring known danger signs – all reflect a deficiency in understanding (or respecting) legal duties. If Dr. Orji and his clinic staff had been well-versed in informed consent laws, they would have known that treating a minor without the guardian’s clear consent is unacceptable and legally risky com. An X-ray is standard of care for fractures; skipping it not only breaches medical protocol but also could be seen as negligent by legal standards, something a legally literate practitioner would be mindful of. Most glaringly, failing to respond to the patient’s “complaints of severe pain” by removing a restrictive cast was a breach of the duty to do no harm thisdaylive.com. Legal literacy training would impress upon healthcare workers that ignoring a patient in distress can constitute gross negligence, as the court indeed found. Moreover, a doctor with proper legal awareness would understand the importance of staying within one’s scope of practice – Dr. Orji was not an orthopaedist, and a legally conscientious doctor might have referred the case to a specialist or sought expert help, knowing that mismanagement could lead to liability. This case also highlights the need for practitioners to know about patients’ rights to quality care and safety; had Dr. Orji centered the patient’s right to appropriate treatment, he might have acted differently. In sum, instilling legal literacy – knowledge of malpractice law, consent requirements, and professional standards – can deter reckless behavior. It empowers providers to make safer decisions (like referring or consulting in difficult cases) and to prioritize patient welfare, thereby avoiding the kind of irreversible harm that befell this patient.
Avoidable Litigation and Reputational Costs: While this case primarily involved criminal prosecution (with the state taking action against the doctor), it carries broader lessons on costs and reputation in the health sector. For one, the case became national news in Nigeria, portraying the medical profession in a harsh light – headlines about a doctor’s jail term for negligence are jarring and can shake public faith. The government of Lagos State invested considerable effort to prosecute Dr. Orji, signaling its commitment to patient safety, but also reflecting that regulatory failures led to this point. If the healthcare system had effective peer review or complaint resolution mechanisms, perhaps the issue would have been addressed before reaching criminal courts. The reputational fallout extends to Nigerian healthcare as a whole: patients might wonder how many other clinics cut corners on safety. Such mistrust is detrimental to UHC efforts, which rely on people feeling confident in seeking care. For the medical community, seeing a colleague convicted was a wake-up call – professional bodies faced scrutiny about why they hadn’t disciplined Dr. Orji earlier (indeed, a medical panel’s previous attempt to suspend him had been tied up in legal challenges com). Thus, the absence of early accountability incurred a much higher cost later: a young patient’s ruined future, a doctor’s career in tatters, and public alarm. All of this could have been avoided had there been a culture of legal compliance and patient-centered care from the start. This case has spurred advocacy in Nigeria for stronger enforcement powers for medical regulators and better negligence laws – for example, calls to empower the Medical and Dental Council to more swiftly prosecute or sanction negligent practitioners healthwise.punchng.com. The hope is that by institutionalizing legal literacy and accountability, such extreme incidents (and their attendant costs) will become rare. It’s far better for a health system’s reputation to correct errors internally and uphold standards than to have courts do it after the fact.
Policy and Training Gaps Exposed: The Dr. Orji saga exposed several gaps in Nigeria’s healthcare regulatory framework and training. A critical gap was in the oversight of private medical practice: Dr. Orji’s clinic was able to handle a complex injury without appropriate expertise or equipment (no X-ray) and apparently without immediate detection by health authorities. This suggests a need for stricter policies on facility licensing, ensuring that clinics only offer services within the competence of their staff and have basic safety capabilities. It also points to a gap in the continuing medical education system – Dr. Orji either lacked knowledge in managing fractures and compartment syndrome, or willfully ignored it. Ensuring that all practitioners undergo regular training (including legal aspects like consent and malpractice) is essential. The case also revealed weaknesses in the accountability mechanisms prior to criminal action. Patients’ families might not know where to lodge complaints about poor care, or perhaps did complain with no timely action, forcing escalation to court. Strengthening patient complaint units and medical disciplinary panels could address issues earlier. In terms of training, this case has underscored the need to incorporate modules on medical law, ethics, and patients’ rights in medical training and licensing exams. A more legally-aware practitioner would know that a simple act like ignoring a patient’s pain can meet the legal definition of recklessness. Finally, this case is prompting policy discussions in Nigeria about balancing patient protection with support for healthcare providers – for instance, introducing clear clinical guidelines (like mandatory imaging for fractures, protocols for treating pediatric patients, etc.) and ensuring practitioners are aware that deviating without justification can have legal repercussions. By closing these policy and training gaps, the health system not only protects patients but also protects well-meaning clinicians from making career-ending mistakes, thereby contributing to a safer and more trusted healthcare environment under UHC.
South Africa: Treatment Action Campaign (TAC) – Right to HIV Medication as a Component of UHC
Background & Outcome: One of the most famous health rights cases in Africa is the Treatment Action Campaign (TAC) vs Minister of Health case in South Africa, which linked legal literacy and activism directly to Universal Health Coverage outcomes. In the early 2000s, South Africa was battling a severe HIV/AIDS epidemic. A breakthrough intervention to reduce mother-to-child transmission of HIV was the drug Nevirapine, which could greatly lower the chance of an HIV-positive mother passing the virus to her newborn. The South African government, however, adopted a restrictive policy: it offered Nevirapine only at a limited number of pilot sites rather than making it broadly available in public hospitals and clinics orgglobalhealthrights.org. No clear timeline was set for scaling up access, meaning that in most parts of the country, pregnant women in the public sector could not get this lifesaving medication. In 2001, the Treatment Action Campaign (a civil society group) sued the government, arguing that this policy violated the constitutional rights to health and to life – specifically Section 27 of the Constitution (the right of everyone to have access to health care services) and Section 28 (children’s right to basic health care and protection) globalhealthrights.org. The Pretoria High Court agreed with TAC, finding that the government’s failure to take reasonable steps to make Nevirapine available violated the Constitution globalhealthrights.org. The court ordered the state to devise a comprehensive program to prevent mother-to-child transmission and to lift the restrictions so that any public facility with the capacity could provide Nevirapine to HIV-positive mothers globalhealthrights.orgglobalhealthrights.org. The government appealed, but in July 2002 the Constitutional Court of South Africa unanimously upheld the lower court’s decision library.law.utoronto.caglobalhealthrights.org. The Constitutional Court acknowledged the state’s duty to act reasonably to save lives within its resources, stating that it was not acceptable to “wait until the best possible program was developed before expanding it,” thereby denying women and children access in the meantime globalhealthrights.orgglobalhealthrights.org. The Court noted that providing a single dose of Nevirapine was a “simple, cheap, and potentially lifesaving” measure well within the government’s means globalhealthrights.org. It ordered the government to remove the policy restrictions and implement a national program to roll out the drug and related services as part of its obligations under the right to health globalhealthrights.orgglobalhealthrights.org. Following the judgment, the South African government rapidly expanded access to Nevirapine and, in the broader sense, it marked a turning point towards scaling up antiretroviral treatment nationally. This case has become a landmark in global health law, illustrating that courts can enforce socio-economic rights and shape health policy to align with UHC objectives.
Preventable Through Legal Literacy: The TAC case underscores that if health policymakers and leaders had better legal literacy (and perhaps fewer ideological blinders), the costly court battle might never have been necessary. Essentially, high-level officials failed to recognize the legal imperative to use available resources to save lives. With greater awareness of constitutional obligations, the Health Ministry might have understood that restricting access to an available HIV prevention drug – without a strong justification – was likely to be deemed unreasonable and unlawful by courts orgglobalhealthrights.org. Legal literacy in this context means appreciating that the right to health imposes an obligation to take prompt, reasonable action when lives are at stake. Had the ministry’s advisors been more attuned to human rights law, they could have crafted a compliant policy (for example, a quicker phased rollout with clear targets) that balanced practical considerations with rights – or at least engaged with TAC and experts in a dialogue rather than a standoff. Moreover, better understanding of administrative law might have shown officials that courts would scrutinize the rationality of their decisions: the government’s concerns (about Nevirapine’s efficacy, resistance, and administrative capacity) were ultimately found to be “unwarranted or hypothetical” globalhealthrights.org, concerns that a more legally and scientifically informed leadership could have addressed without litigation. At the provider level, legal literacy empowers healthcare workers to advocate within the system. During the stalemate, many doctors and provincial health officials knew the policy was flawed; had they known how to invoke patients’ legal rights, they might have pushed back more forcefully. Indeed, the success of TAC’s campaign was partly due to health professionals and activists leveraging legal arguments. In short, if the health system’s decision-makers were as literate in rights and law as the activists were, the crisis might have been solved through policy change rather than court orders. The case demonstrates that integrating legal literacy – understanding that health policies must meet human rights standards – is essential to achieving UHC, because it guides leaders to make decisions that uphold access and equity from the start.
Avoidable Litigation and Reputational Costs: The litigation and delay in the TAC case came at a high price – both human and financial. During the years of government resistance, thousands of infants were born with HIV who could have been protected by timely access to Nevirapine. This human cost is immeasurable, and it starkly illustrates how denying care leads to outcomes that UHC is meant to prevent. From a governmental perspective, the legal fight through multiple courts consumed resources and put South Africa in a harsh global spotlight. At the time, the South African government (under President Thabo Mbeki’s administration) faced international condemnation for its hesitancy in rolling out HIV treatments. The reputational damage was severe: South Africa’s health policy was portrayed as being guided by denialism and neglect of evidence, undermining the country’s leadership role in public health. Internally, public trust in the health system was shaken – TAC’s victory, while positive, highlighted that citizens had to drag their government to court to get basic interventions, which is not a good look for a country committed to equitable healthcare. If the officials had heeded legal and moral arguments earlier, they could have avoided being seen as adversaries to their own people’s health. After the court ruling, the government not only had to expand the program under scrutiny but also had to catch up on broader antiretroviral treatment efforts, eventually rolling out one of the world’s largest HIV treatment programs (an outcome that could have started sooner). On the positive side, the case’s publicity did mobilize public support for UHC principles – it educated many South Africans about their health rights and the power of legal action, which is a form of increased legal literacy in society. However, relying on court battles to settle such issues is inefficient and adversarial. The TAC case teaches governments that baking legal compliance into health policymaking from the outset is far preferable. It saves the costs of litigation, protects the country’s reputation, and most importantly, saves lives by implementing UHC measures without undue delay.
Policy and Training Gaps Exposed: The TAC litigation exposed a policy gap in how South Africa initially approached UHC for HIV prevention. The government’s cautious pilot-only policy revealed a disconnect between public health evidence and the state’s obligations – essentially a lack of a rights-based approach to policy. Post-case, there was a clear need for policy reform: to explicitly acknowledge that life-saving medicines (once proven effective and affordable) should be made widely accessible as part of the state’s duty to progressively realize the right to health. This case catalyzed the integration of human rights norms into health policy – for example, South Africa’s subsequent HIV/AIDS plans were framed around the rights to treatment and prevention, ensuring that policy goals aligned with constitutional mandates. On the training side, the case highlighted that not only health workers but also health administrators and policymakers need education in health law and human rights. The reluctance of some officials stemmed partly from misinformation and lack of legal perspective; thus, training programs for health executives now often include components on the legal context of health (constitutional rights, health ethics, etc.). Another gap was the lack of community legal literacy before TAC’s intervention – many patients were unaware they could demand such services. TAC filled that gap by spreading awareness, an approach that could be institutionalized via patient charters and legal empowerment initiatives in the health system. Finally, the case underscored the importance of accountability mechanisms: it set a precedent that policies can be reviewed by courts for reasonableness. In effect, it taught both the public and officials that UHC isn’t just a political promise but a legal commitment. The lesson for policy-makers is to routinely evaluate health policies against constitutional standards (e.g. is this policy equitable? Are we using maximum available resources for health?). Incorporating those checks, and training officials to think that way, is a lasting improvement spawned by the TAC case. In summary, the TAC case reinforced that legal literacy and respect for rights must guide policy and training if UHC is to be achieved – health systems must plan not only for clinical effectiveness but for legal and ethical soundness.
Uganda: CEHURD v Attorney General – Maternal Health Rights and System Accountability
Background & Outcome: In Uganda, a groundbreaking case brought the issue of maternal mortality and health system failures into the courts, illustrating how legal action can promote accountability for UHC-related goals. In 2011, the Center for Health, Human Rights and Development (CEHURD) and families of two women who had died in childbirth (Sylvia Nalubowa and Jennifer Anguko) sued the Ugandan Government (Attorney General), arguing that the government’s failure to provide essential maternal health services violated the women’s constitutional rights com. Uganda at the time had a very high rate of maternal deaths – more than 16 women dying daily from mostly preventable causes theguardian.comtheguardian.com. The two specific cases were emblematic: one woman died because she could not access a blood transfusion in time, another died after hours of unattended obstructed labor – tragedies traceable to systemic neglect (lack of supplies, inadequate staffing, and poor emergency response) theguardian.com. The petitioners claimed that such conditions infringed the right to health, the right to life, and the rights of women to dignity and equality. Initially, in 2012, the Constitutional Court of Uganda dismissed the case on a technicality, controversially ruling that it was a “political question” outside the court’s authority to decide health policy theguardian.comtheguardian.com. This dismissal provoked public outrage among civil society, as it appeared to shut the door on judicial relief for the crisis in maternal health. CEHURD and the families appealed to Uganda’s Supreme Court. In a landmark Supreme Court ruling on 30 October 2015, the dismissal was unanimously overturned theguardian.com. The Supreme Court held that the Constitutional Court did indeed have the mandate (and duty) to hear the case on its merits, and that it must determine whether the government’s inaction on maternal healthcare constituted a violation of constitutional rights theguardian.comtheguardian.com. The Chief Justice emphasized that courts cannot shy away from adjudicating socio-economic rights issues when lives are at stake. This decision was hailed as a huge victory by activists – effectively, it meant the judiciary recognized that preventable maternal deaths could indicate a breach of the state’s obligations. The case (often referred to as “Petition 16 of 2011”) was sent back for a full hearing on its merits in the Constitutional Court. In the years following, the mere prospect of that hearing prompted some government action: for example, after the case was filed, Parliament approved an unprecedented 49.5 billion Ugandan shillings in extra funding to recruit midwives and health workers, an allocation credited to the pressure from the lawsuit theguardian.comtheguardian.com. Eventually, in 2020, Uganda’s Constitutional Court heard the case and in 2021 it delivered a judgment (not available in the excerpt above, but widely reported) finding that the government’s failure to provide basic maternal care (like emergency obstetric services and commodities) violated the right to health and the right to life. The Court recommended remedies including increased budgetary allocations to maternal health and better oversight of health facilities. In essence, CEHURD v AG became a catalyst for greater accountability in Uganda’s health system and established that maternal health is a justiciable right.
Preventable Through Legal Literacy: The maternal deaths at the heart of this case were not caused by unknown diseases or unforeseeable events – they were the result of health system lapses that could have been prevented if individuals and officials at various levels had been more aware of their legal responsibilities to patients. At the clinical level, improved legal literacy among healthcare workers could empower them to advocate for patients in critical moments. For instance, if a hospital nurse knows that a woman in obstructed labor has a right to emergency obstetric care, she might be more inclined to escalate the situation to hospital management or even to call in a higher authority when a doctor is not available. In one of the tragic cases, a woman’s relatives were reportedly asked to pay for fuel in an ambulance and to buy blood from a private facility – delays that led to her death com. A health worker informed about patients’ rights and state obligations might have refused to let such hurdles impede urgent care, perhaps by invoking the hospital’s duty to provide emergency treatment regardless of payment (a policy many countries have, but often not enforced). Additionally, front-line providers with legal awareness would understand that every maternal death is a potential legal liability – this creates an impetus to follow protocols, document complications, and not neglect a patient in distress. In Jennifer Anguko’s case, she allegedly bled to death unattended on a hospital floor; no one should have to fear legal repercussions to simply not leave a patient unattended, but awareness that such neglect could amount to a rights violation might compel staff to double down on vigilance. At the administrative level, legal literacy means recognizing that government officials can be held accountable for systemic failings. If district health officers or ministry personnel were cognizant that not supplying basic needs (like blood, oxytocin, or sufficient staffing) could breach constitutional rights, they would be more proactive in allocating resources and fixing gaps. Essentially, treating maternal health as an enforceable right – which it now clearly is in Uganda – changes the mindset from “charity” to “obligation,”and that mindset needs to permeate to every health worker. Legal literacy training can inculcate that attitude: for example, including modules on human rights in maternal health in midwifery and medical education, so providers see themselves as duty-bearers for those rights. In summary, if the health workers and managers in these cases had been legally literate, they might have acted differently (faster referrals, no demands for unofficial fees, constant care) out of an understanding that failing to do so wasn’t just unfortunate – it was unlawful.
Avoidable Litigation and Reputational Costs: The Ugandan government’s initial response to the maternal mortality crisis – essentially defending the status quo in court – ended up backfiring in terms of reputation and cost. The litigation spanned a decade, attracting critical domestic and international attention. Uganda found itself in the news not for improvements in maternal health, but for fighting bereaved families in court. This adversarial posture was damaging: it gave the impression that the government was indifferent to the plight of dying mothers, which is a public relations and moral nightmare. The drawn-out legal battle also meant continued legal expenses and the opportunity cost of not addressing the core issues sooner. When the Supreme Court reversed the dismissal in 2015, civil society hailed it as a victory for all Ugandan women comtheguardian.com, implicitly painting the government as having been on the wrong side of justice until then. Politically, the case coincided with election cycles, forcing maternal health onto the agenda; while that had positive outcomes (like campaign promises and the aforementioned emergency hiring of health workers), it also meant the government was pressured under public scrutiny rather than acting in a planned, proactive manner theguardian.comtheguardian.com. From a UHC perspective, the trust between citizens and the state was eroded – people saw the courts, not the health ministry, as the champion of their health rights. This dynamic is not ideal for a sustainable health system; governments would prefer to be seen as willingly upholding health rights, not yielding only when courts compel them. All of these costs – legal, reputational, political – could have been largely avoided if the health system had acknowledged the problem and addressed it without litigation. Had there been an earlier recognition by officials that “yes, we have a legal and ethical duty to drastically cut maternal mortality,” they might have initiated reforms (e.g. increasing funding, improving facilities) pre-emptively, possibly rendering the lawsuit unnecessary. The lesson here is that embracing legal accountability early spares the state the embarrassment and expense of being forced into action later. Notably, since the case, Ugandan authorities have shown more openness to dialogue on health rights, and maternal health indicators have modestly improved with sustained investment – steps that came after the legal reckoning. In essence, preventive legal responsibility is better than post-hoc legal battles for all involved.
Policy and Training Gaps Exposed: CEHURD v AG illuminated several critical gaps in Uganda’s health system that are common in many settings. A glaring gap was the lack of a formal accountability framework for maternal health. Prior to this case, maternal deaths were often seen as unfortunate but not as triggers for any governmental review or action. The legal proceedings helped introduce the idea of a maternal death audit as not just a health best-practice but a potential legal necessity – if a pattern of neglect is shown, someone could be held liable. Policy-wise, this has pushed Uganda toward strengthening maternal death surveillance and response (MDSR) systems. Another gap was in budgetary priority: the case exposed that the health sector (especially maternal health) was under-resourced (at one point Uganda was spending a very low percentage of its budget on health, contrary to Abuja Declaration targets com). The attention from the case spurred a one-time budget boost and has since kept up pressure for sustained funding. In terms of training and systemic culture, the case showed a deficiency in how health workers and administrators are oriented toward patient rights. The fact that families had to pay bribes or that women were left unattended points to a culture of normalization of substandard care. To change this, Uganda and countries like it have been prompted to integrate human rights-based approaches into health worker training – for example, emphasizing respectful maternity care, which includes never abandoning a woman in labor and ensuring informed consent for all interventions. Additionally, the legal process itself became a learning opportunity: it educated not just the public but also many officials and health workers that courts can and will review health failures. This has led to a subtle but important shift: health policies and programs are now sometimes reviewed by legal experts or framed in rights-based language to pre-empt challenges. For instance, Uganda’s later health sector plans made reference to equity and rights, and the Ministry of Health worked with human rights groups to develop a Patients’ Charter. These are direct or indirect outcomes of the policy and training gaps that the CEHURD case highlighted. Ultimately, filling those gaps – through better-funded services, training in legal responsibilities, and creating channels for accountability – strengthens the health system. It ensures that universal health coverage is not just about infrastructure or financing, but also about a system that is responsive and answerable to the people it serves.
CONCLUSION
Each of the cases above – spanning different countries and aspects of healthcare – arrives at the same conclusion: when healthcare systems lack legal literacy and accountability, patients suffer preventable harm and the lofty goals of UHC are undermined. Conversely, integrating legal knowledge and respect for rights at all levels of the health system creates a safer, more trustworthy environment that brings us closer to true universal health coverage. Legal literacy empowers healthcare workers to obtain informed consent, respect patient choices, diligently follow standards, and document their care, knowing that these are not just medical niceties but legal obligations tied to patients’ fundamental rights. It also equips health administrators and policymakers to design and implement health services that meet the tests of equity and justice, thereby avoiding court battles and public outrage. The cases of Theonistar /Naris, LM in Namibia, Helena Nyamekye, Dr. Orji, TAC, and CEHURD v AG all illustrate failures that might have been averted with better understanding of the law and proactive compliance. They show that legal empowerment in health is not an abstract concept – it translates into very tangible outcomes: a woman not sterilized against her will, a mother surviving childbirth, a child keeping his limb, or a baby being born HIV-free. These are the human faces of UHC’s promise, and legal literacy is a missing pillar that can help fulfill that promise. Strengthening this pillar means updating curricula, running continuous training on medical ethics and law, enforcing clear policies on patient rights, and fostering a culture where accountability is embraced rather than feared. Doing so not only prevents tragedies and lawsuits but also builds public trust that the health system will “do no harm” and will remedy any wrongs. In the journey toward UHC, countries must recognize that health without justice is incomplete – quality and coverage must go hand in hand with rights and accountability. Legal literacy bridges that gap, ensuring that universal health coverage truly includes universal respect for patient rights and dignity.
SOURCES
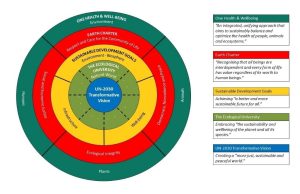
The WHO’s recent decision to consider anti-obesity drugs as essential medicines occurs in a world marked by profound contradictions: persistent global undernutrition, widespread overconsumption, accelerating ecological degradation, and unprecedented corporate concentration in the agri-food and pharmaceutical sectors. Industrial food systems generate vast ecological harm and animal suffering while driving both obesity and hunger. This article analyzes the ethical, ecological, and equity implications of medicalizing obesity, drawing on global health ethics, political ecology, and the author’s earlier work on sustainable health equity, as well as the principles articulated in the Sustainable Health Equity Movement (SHEM) webinars. It argues that pharmaceuticalizing a structurally produced problem risks perpetuating an economy of excess—of calories, material throughput, wealth accumulation, and ecological destruction—while deflecting attention from the structural transformations needed to achieve equitable and sustainable global health