Labour migrants in Russia unfortunately still have lack of access to health services. They also face a lot of barriers to a normal life from government and society in common.Daniel Kashnitsky, a junior researcher at the Higher School of Economics on direction on labour migration and HIV positive migrants living in Russia, told AFEW International about migrants’ medical insurance, collaboration with Russian authorities and some hopes for the better future
AFEW International intern
AFEW is dedicated to improving the health of key populations in society. With a focus on Eastern Europe and Central Asia, AFEW strives to promote health and increase access to prevention, treatment and care for major public health concerns such as HIV, TB, viral hepatitis, and sexual and reproductive health
Labour Migrants in Russia and their Needs
Which difficulties do labour migrants from Central Asia face in Russia?
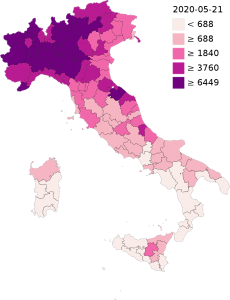
It depends on a country where these migrants come from. People from Kazakhstan and Kyrgyzstan feel a bit better in Russia, because those countries are part of the Eurasian Economic Union. Citizens of those countries do not need to apply for a residence permit nor for the permit to work. They can just come and only need to have an official registration in the place where they live. To get this document might become a barrier for some people, because not all the landlords are ready to provide them with an official registration.
Also, some migrants are eligible to apply for the state medical insurance. Migrants from Belarus, Armenia, Kyrgyzstan and Kazakhstan have been eligible to have one since three years ago, however TB and HIV services are not included in this state medical insurance.
But there are countries, such as Uzbekistan and Tajikistan, who are not part of the Eurasian Economic Union. Migrants from there have to apply for work permits, and they have to reapply every year. They also have to pay a special tax every month, which is a really heavy burden considering the low wages. It’s a large part of their income, so it affects them enormously.
Also, migrants can face some other issues. For example, in the Russian Federal law number 38 there is a paragraph saying that if a foreign citizen is identified with HIV or TB he/she needs to be deported from the country. If one is identified with HIV and it is known by the migration authorities, they will include the migrant’s name in their database. Since deportation is quite expensive, migrants often remain in Russia undocumented. But if once you leave Russia, you will be banned to re-enter. There is a small part of undocumented migrants who had been caught and they are kept in those detention centres. Other migrants live in hiding and keep working, doing black jobs. Some of them get ART (antiretroviral therapy) in NGOs and private clinics, however a large part of them do not have access to health services, they just keep living as their CD4 level goes down, and some of them they just end up in the emergency care. Unfortunately, we cannot estimate the figures, because the undocumented migrants are not in the state statistics or the patient file data.
What are the factors that influence a lack of access to health services for labour migrants? Probably language barriers, or something else?
Speaking the same language is important of course, because talking about health and body is quite intimate. People prefer to not only speak in their native language, but also to speak to a person who understands them, their social determinants of health, the culture.
Some migrants from Central Asia explained me why they prefer to go to clinics where people of their culture work. One of the reasons was that migrant doctors better understand socio-economic circumstances of migrants’ experiences in Russia. For example, they tend not to prescribe expensive medicines, because they know that migrants cannot afford them. One of the biggest barriers is discrimination in clinics and state institutions. Migrants from Central Asia are often exposed to it.
Unfortunately, migrants can be a reason of rising HIV epidemic in their countries, don’t they?
True. The migration of Central Asia is predominantly male, 80% of the migrants from Central Asia are young males from 20 – 50 years old. They are mostly seasonal migrants. They go to Russia for 10-11 months a year, then they go back to their home country for one or two months. This is the only time when they get to see their wives, children, and other relatives. A lot of them have sexual intercourse in Russia (sometimes not safe), with sex workers, or just with female from their communities.
What have you and your organization done to address the issue of labour migrants having a lack of access to health services?
First of all, me and my colleagues created a regional expert group on migration health in our region. It’s an informal network of civil society experts. We are trying to collect arguments and convince policy makers to lift the residence ban for HIV positive foreign migrants in Russia. We are trying to bring evidence to decision-makers that the HIV residence ban only aggravates the epidemiologic situation. It creates negative consequences for the migrants as they can spread the virus even further to the community. It affects a lot of people as they spread it in their home country. We have been in dialogue with the Russian authorities about this, but it is a long process to create this enabling atmosphere and to actually make it happen.
So, it’s hard to collaborate with the Russian authorities, isn’t it?
Yes, because the Russian authorities are little sensitive now to what civil society is claiming. You need to have very strong argument, create a supportive environment and change the public opinion. We are working with the journalists. We helped to create lot of publications on migrants with HIV living in Russia. We work with civil society organizations and we train them. Our partner organizations have direct services for migrants, at least in Moscow, St. Petersburg. Yekaterinburg and Rostov-on-don and some other large Russian cities that attract them labour migrants.
Some limited services for migrants do exist where they can get tested for HIV, where they can have consultations. But it is difficult to provide sustainable provision of ART, and this is a large problem as most of the migrants cannot afford therapy.
Today the Russian government seems reluctant to introduce any serious changes. On one hand, the authorities understand that Russian economy would not survive without migrants. So, they try to keep migrants low profile. They do not encourage migrants to raise their voices, to create trade unions or other grassroots movements. Migrants do not have access to social entitlements, not only healthcare but to pension funds and other security funds.
What do you think should be done by the Russian government to improve the access to health services for migrants from Central Asia?
The first thing Russia needs to do, is to liberalize its HIV legislation. This is very important, because once HIV-positive migrants are not stuck in Russia, then they can travel back and forth, at least they can receive ART from their home country. Secondly, Russia needs to allocate funding for NGOs that work with the migrants, to test them and provide psychosocial support. Third, anyone who resides in Russia and contributes to the Russian economy, should get access to the Russian healthcare, including HIV and TB services. The healthcare needs to change and include all the people who actually live and work in Russia. There is a human right aspect here, but also an epidemiological aspect: if you don’t want the diseases to spread further, you need to provide basic access to services.
How do migrants from countries like Tajikistan, Uzbekistan get health insurance in Russia?
They don’t have access to state insurance. But one of the requirements when applying for a work permit, is to have bought a private healthcare insurance. They can buy it from one of the private insurance companies. And it is a very basic insurance scheme, that costs about 50 euros per year. It is meant to show the authorities that one is formally secured, but in fact it does not improve with access to health care. These minimal insurance packages provide almost nothing more than just free emergency care which is still provided free of charge to anyone physically residing in Russia. If you have broken your leg or if you have any other acute situation, you will receive emergency care as it is accessible to anyone in Russia. But if you need any further treatment, then you need to pay. And in most cases the basic private insurance will not help you. Of course, you can buy a more expensive one, that would include everything, but most of migrants cannot afford it.
Do you see an opportunity that the situation will be changed in the future?
Well, I stay positive because there are some developments in the region of East Europe and Central Asia such as, for example, Kyrgyzstan and Kazakhstan having accessed to the Eurasian Economic Union. It was a major breakthrough, when member countries signed a health insurance agreement to cover their citizens when they migrate within the Union. In terms of access to HIV and TB care, it really has remained unchanged for 25 years, because when they adopted these policies, Russia did not have this severe HIV growth that it has now, it was only starting back then.
Nowadays we try to tell the authorities: it is not that you have to pay for the migrants and their health insurance, but just start with decriminalizing them, liberate migrants from this constant fear of being deported, of residing in illegality and being constantly subject to rights violation. This is really important if Russia ultimately wants to be created decent life conditions for all people who live and work in the country.