‘The concern about access, so far, has not yet been incorporated into research for treatments or vaccines for COVID-19, despite significant pressure from civil society’.
The several years of indifference to the reality of people affected by neglected diseases seem to have created one of the greatest obstacles to the coronavirus pandemic control. By accepting that new health technologies were determined by Big Pharma's economic interest at the expense of millions of people’s lives, we’ve naturalized our lives pricing and the understanding of health as a commodity - and an expensive one! So now we are forced to ask ourselves: when the coronavirus vaccine comes out, will my family and I have access to it? Will we and our health systems be able to buy the drug?
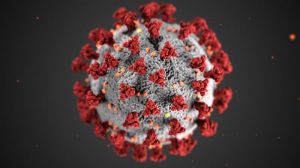
image credit: Centers for Disease Control and Prevention (CDC)
By Luciana M. N. Lopes and Alan Rossi Silva*
Translated by Luciana M. N. Lopes and Alan Rossi Silva
Originally published at Le Monde Diplomatique Brasil
Diseases Are Neglected by the Pharmaceutical Industry
Another day. Many thoughts I can’t avoid. Do I need to be isolated? Is my family at risk? Will I have any sequelae? Will I lose my job? If so, how’d we live? Will I run out of food? If I go to a hospital, will they look after me? Will someone look down on me on the streets? What if someone gives me some drug? Hasn’t anyone invented a better medicine that can fix one thing without ruining another one? What about this vaccine that hasn’t come out? When is it being launched?
Fear. Anxiety. Anguish. The wait. Many people living with neglected diseases have been dealing with for a long period of time – sometimes for a lifetime, feelings the whole world got to share in recent weeks.
According to the World Health Organization (WHO), every year, around 1.5 billion people (20% of the world population) in more than 140 countries need interventions against Neglected Tropical Diseases (NTDs). We’ve heard of several of them: leishmaniasis, leprosy (Hansen’s disease), Chagas disease, schistosomiasis, among others, which disproportionately affect populations and regions in social vulnerability. These diseases are so called by not being of great interest to the pharmaceutical industry that does not see sufficient economic return to spur its commercial interest for Research and Development (R&D).
Imagine that: you wake up, make a coffee and open the newspaper. A headline pops up: ‘research and development of COVID-19 vaccine is canceled due to lack of economic interest’. It’s true that this scenario seems difficult to imagine. After all, researchers, governments, companies, nonprofits and several other actors are in a race against time to make new technologies available that could change history and the story of the coronavirus pandemic. According to the Milken Institute mapping, there are more than 90 development studies for treatments and more than 50 for vaccines. Every day, a flood of news has been published on the subject, and apparently, we’re getting closer to a solution for this new disease.
Quickness
A quick launch of a vaccine or a proper treatment against COVID-19 would make all our lives easier, but especially lives of people like Nancy Dominga: ‘I’m between my life and my job. And between my life and my job, I’ll pick my life and I’ll stay at home’. She is in a risk group for COVID-19 because she has heart issues – sequela of a disease that hasn’t been controlled in many parts of the world, despite being around for 111 years: Chagas disease.
Like COVID-19, many NTDs affect entire families. Nancy lost four beloved ones to Chagas disease, which kills around 14,000 people a year in Latin America. There are between 6 and 7 million infected people in the region, but less than 10% of them are diagnosed and less than 1% receive treatment at the appropriate time. There is no vaccine. And both available drugs are over 50 years old, have efficacy limited to early stages of the disease and show relevant adverse effects.
We’re all worried about our grandparents, parents, uncles, aunts, friends and colleagues who are in a risk group for COVID-19. We want society to get mobilized and provide social and economic conditions so our loved ones can stay at home and have no need to expose themselves to be at risk of infection. So, can you imagine knowing that someone you love is in a risk group precisely because she or he was exposed to society’s indifference?
This abandonment is historical. There are diseases that are still important today, such as leprosy (there were more than 200 thousand new cases in the world only in 2018), that have caused suffering for – literally – millennia. As if the anguish of waiting for an effective, safe and quality treatment that never comes was not enough, these neglected people often additionally suffer from the prejudice of an ill-informed society.
Neglected diseases
And it was thinking of it that, in 2016, the Brazilian Social Forum to Confront Neglected and Infectious Diseases was created as a collective of movements, organizations and individuals that fight in defense of the right to health of people and communities affected by and/or living with infectious and neglected diseases. Eloan Pinheiro, former director of the Institute of Drug Technology (Farmanguinhos) in Brazil and one of the founders of the Forum, points to the initiative as an important space to share knowledge, combat discrimination and fight for public policies that can change the reality of these people.
She warns us that the struggle for NTDs drugs and for their cure is crucial but not enough: new people will get infected if deeper causes of these diseases, such as poverty and lack of adequate housing, are not addressed. When referring specifically to the need for new NTDs drugs, Eloan invites us to think outside the box: ‘It’s not enough to just have the drugs, it’s necessary to fight for a financial fund to study new products, diagnostic kits and vaccines, using even local knowledge of medicinal plants. It’s necessary to dare leave the traditional Big Pharma product development scheme’.
We need indeed to seek different paths – especially because we’re dealing here with diseases and people which are invisible to our traditional social structures. COVID-19, on the other hand, ‘has a very different profile from neglected diseases regarding its visibility, its presence on the public agenda and the attention it gets of the media’, says Francisco Viegas, the Latin America Advocacy Advisor for a non-profit drug R&D organization for NTDs: the Drugs for Neglected Diseases Initiative – DNDi. Francisco also points out that the fact that COVID-19 reaches rich Countries and ‘in addition to a large market horizont for new health tools, arouses the interest of multiple actors in searching for solutions’.
While in 2018, according to the G-Finder Report, the global funding for basic research and product development for NTDs from 262 entities reached a record amount of US$ 4.05 billion, Johnson & Johnson and the US government alone have pledged to co-invest more than US$ 1 billion in a COVID-19 vaccine R&D. If, on the one hand, knowing that there are several actors – including Big Pharma – in search of technologies for COVID-19 brings some relief, on the other hand, it turns on a warning light: if there’s economic interest in saving my life, how much does it cost?
Access
Having worked for 15 years with a R&D model alternative to the one traditionally adopted by the pharmaceutical industry, Francisco highlights that ‘DNDi considers that its innovative treatments must reach all countries and patients who need them, that’s why we work with the notion of ‘public good’. It means that they ideally have no patent protection and have price affordability guarantees’. Despite the fact that a great number of studies against the new coronavirus has adopted collaborative approaches in order to speed up investigations – just as DNDi usually does -, Francisco warns us: ‘the concern about access, so far, has not yet been incorporated into research for treatments or vaccines for COVID-19, despite significant pressure from civil society’.
The several years of indifference to the reality of people affected by neglected diseases seem to finally collect their debt. All this time we’ve tolerated an unfair incentive system for health innovation may have created one of the greatest obstacles to the coronavirus pandemic control.
By accepting that new health technologies were determined by Big Pharma’s economic interest at the expense of millions of people’s lives, we’ve naturalized our lives pricing and the understanding of health as a commodity – and an expensive one! So now we are forced to ask ourselves: when the coronavirus vaccine comes out, will my family and I have access to it? Will we and our health systems be able to buy the drug?
The good news is that the COVID-19 pandemic, exactly by collecting our debts from the past, is also giving us the opportunity to stop, think, catch up on our obligations and put our house in order. Giving visibility to the reality of people affected by NTDs during the current crisis doesn’t mean to establish a hierarchy among the diseases. It’s quite the opposite. It’s the strong statement that we won’t be able to overcome this challenge if we continue to accept a system that ignores the suffering of millions of people as if they were less valuable and their needs were less urgent.
Epidemics and diseases, regardless of our will, will continue to emerge. What we can change is how we look at those affected by all of them and how we face them. It’s precisely at this moment when humanity is called to fight an invisible enemy that we have the unique opportunity to notice the silenced reality of those who have waited, for a long time, to be seen.
————————————————-
*Luciana M. N. Lopes is a PhD student in Public Health at the Federal University of Minas Gerais (UFMG) and Alan Rossi Silva is a PhD student in Law at the State University of Rio de Janeiro (UERJ), in Brazil. They represent the Universities Allied for Essential Medicines (UAEM), a student-driven organization in defense of universal access to medicines and a fair biomedical innovation system.